Towards biopsy-free monitoring: contrast-enhanced ultrasound perfusion metrics correlate with graft pathology in pediatric kidney transplant recipients
Bernarda Viteri Baquerizo1,2, Tatiana Morales-Tisnés3, Laith R Sultan3, Jarcy Zee2,4, Brenda Laventure1, Tricia Bhatti5, Sandra Amaral1,2, Susan J Back 2,3, Hansel J Otero 2,3.
1Department of Pediatrics, Division of Nephrology, Children’s Hospital of Philadelphia, Philadelphia, PA, United States; 2Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, United States; 3Department of Radiology, Children’s Hospital of Philadelphia, Philadelphia, PA, United States; 4Research Institute, Children’s Hospital of Philadelphia , Philadelphia, PA, United States; 5Division of Anatomic Pathology, Children's Hospital of Philadelphia, Philadelphia, PA, United States
Purpose: Contrast-enhanced ultrasound (CEUS) provides a non-invasive alternative to biopsy for assessing the perfusion of kidney transplant allografts. We compared CEUS parameters with histopathological measures of dysfunction.
Materials and Methods: This prospective, single-center study enrolled pediatric kidney transplant recipients aged 6 to 21 years undergoing clinically indicated biopsies from Nov 2020 to Sept 2024. Patients who consented and had no contraindications for CEUS were included. CEUS imaging was performed within 48 hours prior to biopsy. After intravenous administration of ultrasound contrast agent (0.03 mL/kg) a 2-minute cine loop of the transplanted kidney was performed. Four parenchymal regions of interest (ROI) were identified in post-processing using Interactive Data Language (IDL) software. IDL depicted the CEUS parameters for each ROI over time: mean transit time (MTT), time to peak (TTP) and peak enhancement (PE). Perfusion index (PI) was calculated. The ROI values were compared to three histopathologic outcomes per Banff 2017 criteria: chronic allograft damage index (CADI) score, rejection, and total inflammation (ti), which was categorized as 0 vs. 1-3. A generalized estimating equations model was used to account for repeated measures.
Results: Forty CEUS examinations were performed; two were excluded due to incomplete clips, leaving 39 exams from 28 subjects (75% male) for analysis. The median age at the time of CEUS was 16 years (IQR: 6). The mean estimated glomerular filtration rate was 68.9 mL/min/1.73m² (IQR: 20.3), and the median time from transplant to biopsy was 14 months (IQR: 23). Median CEUS parameters were as follows: TTP 12.7 seconds (IQR: 17.6), MTT 57.1 seconds (IQR: 41.2), PE 136.3 a.u. (IQR: 29.3), and PI 27.59 a.u. (IQR: 1.52). The median CADI score was 2 (IQR: 2), with 26 out of 39 biopsies (66.7%) showing a ti score of 0, and rejection detected in 15 biopsies (38.5%). TTP was significantly associated with CADI score (β = 0.05, p = 0.013). MTT was significantly associated with both CADI (β = 0.37 per 10 seconds, p = 0.002) and ti score (OR = 1.51, p = 0.013). PE was also significantly associated with CADI score (β = 0.02, p = 0.048).
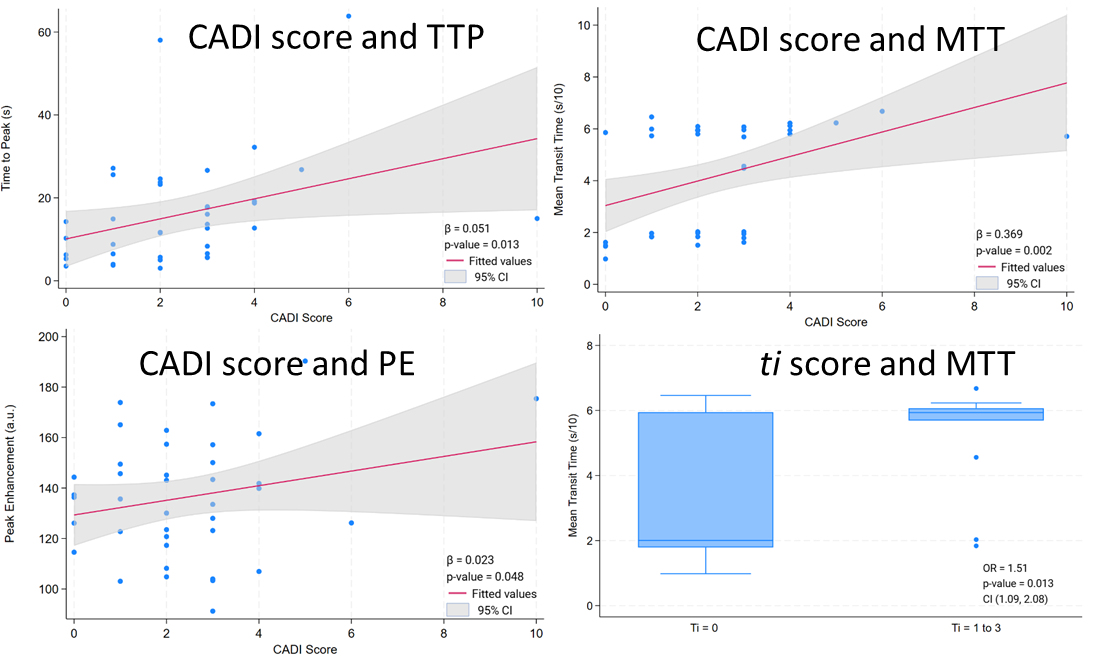
Conclusion: We demonstrated that as CEUS-derived perfusion parameters, specifically mean transit time, time to peak and peak enhancement increase, CADI also does. Mean transit time was also strongly associated with increasing inflammation, indicating that slower blood flow through tissue is linked to both greater damage and inflammation. These findings suggest that CEUS may play a role as a non-invasive tool for early detection of allograft dysfunction.
[1] Allograft Survival
[2] Kidney Imaging
[3] Ultrasound