Split liver transplantation using machine perfusion in pediatric recipients
Amanda Jensen1, Toshi Nakayama1, Kliment K Bozhilov1, Varvara Kirchner1, Noelle Ebel1, Marc Melcher1, Kazunari Sasaki1.
1Division of Abdominal Transplant Sugery, Stanford Health Care, Palo Alto, CA, United States
Purpose: Due to the size discrepancy between donors and recipients, pediatric liver transplant recipients often require a technical variant graft. Machine perfusion (MP) with sequential ex vivo split transplants may enable pediatric recipients to receive split grafts from distant donor centers. This study evaluated the current trends and outcomes of split liver transplantation (SLT) combined with MP.
Methods: A retrospective cohort review of the United Network for Organ Sharing database was conducted for all SLT cases between January 2022 and December 2024. Eight recent cases without available machine perfusion data were excluded. Graft and patient survival outcomes were compared between recipients who underwent SLT following standard cold storage (SCS) and those who received SLT with MP (MP+SLT). Donor cross-clamp time to liver reperfusion in the recipient was calculated as "preservation time" (PT).
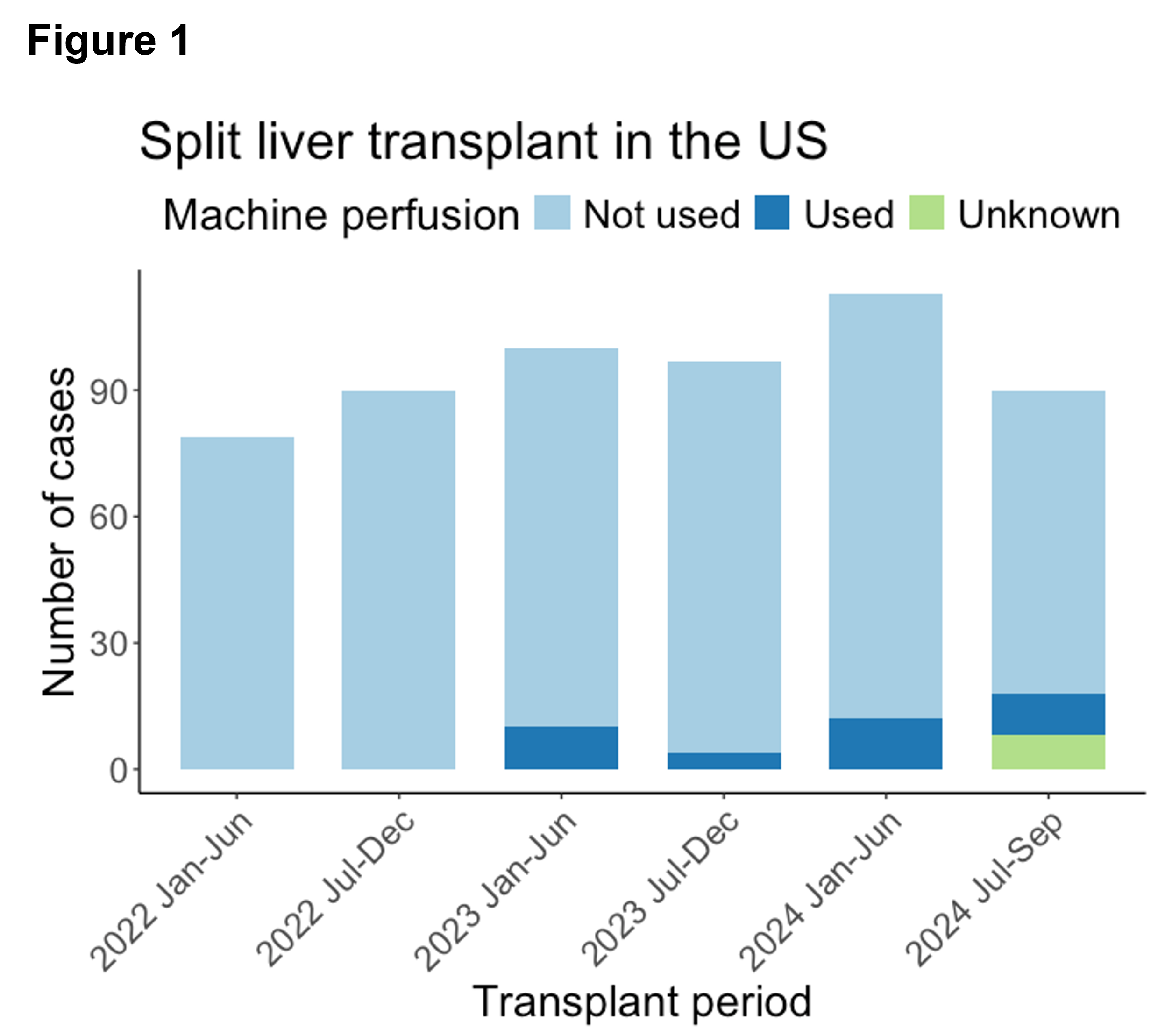
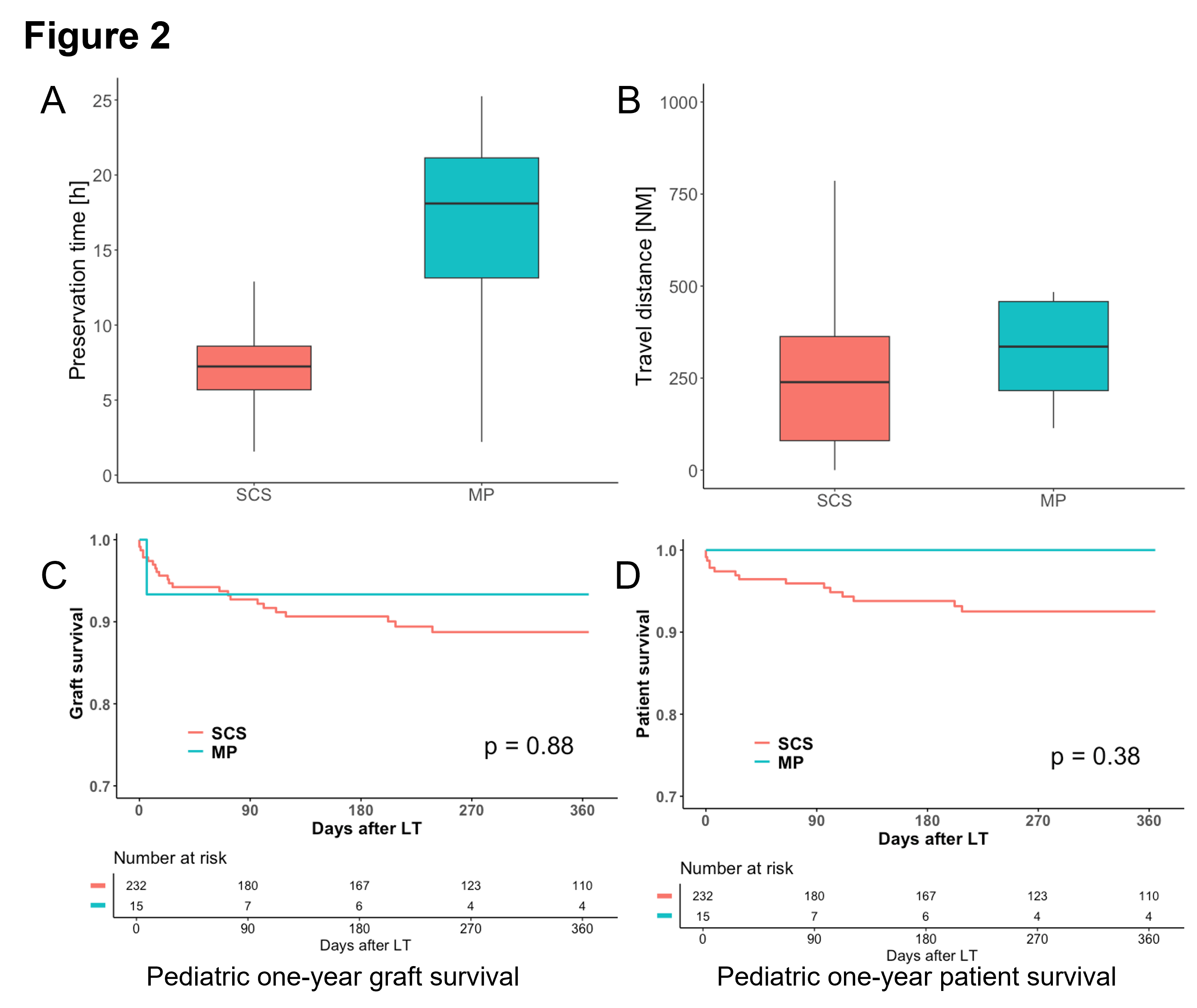
Results: A total of 569 SLT cases were identified during the study period, of which 36 involved MP (32 normothermic MP, 2 hypothermic MP, and 2 unspecified). The remaining 525 SLT cases were performed without MP (Figure 1). MP was utilized in adult/adult (2 pairs), adult/pediatric (15 pairs), and pediatric/pediatric (1 pair) transplant combinations. When MP was used, the same transplant center utilized both graft variants in 94.4% of cases, a significantly higher proportion than non-MP SLT (61.4%, p < 0.01). The median distance between donor and recipient centers was significantly greater in the MP+SLT group (393.5 NM) compared to the SCS+SLT group (240.0 NM, p < 0.01; Figure 2B). The median PT was 18.1 hours in the MP+SLT group versus 7.2 hours in the SCS+SLT group (p<0.01, Figure 2A). In pediatric SLT, there was no significant difference in graft survival (93.3% vs. 88.7%, p = 0.88) or patient survival (100% vs. 91.8%, p = 0.38) at one year between the MP+SLT and SCS+SLT groups, respectively (Figure 2C and 2D).
Conclusion: Machine perfusion prior to SLT is technically feasible and safe. While still in its early stages regarding experience and volume, MP facilitates pediatric transplant centers acquiring organs from distant donor centers without compromising one-year post-transplant outcomes. MP has the potential to transform clinical practice in pediatric SLT, improve logistics, and enhance organ utilization.
Stanford Transplant Outcomes Research Center.
[1] machine perfusion
[2] liver transplant
[3] technical variant
[4] split graft