
CD4 counts exhibit poor recovery in pediatric transplant patients with single ventricle physiology
Brian Madden1, Rachel Osoba2, Caitlin Li2, Ravi Jhaveri2, Aisha Ahmed3, Taylor Heald-Sargent2.
1Cardiology, Ann and Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; 2Infectious Disease, Ann and Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; 3Allergy and Immunology, Ann and Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States
Introduction: While induction and maintenance immunosuppression improve graft survival, especially in heart transplant patients, their long-term effects on the immune system remain poorly understood. Prior studies demonstrate different immune phenotypes before transplant and changes in flow cytometry from before to after transplant in kidney transplant patients, and in heart transplant recipients for congenital heart disease (CHD) and single ventricle (SV) physiology, but most patients receive standardized immunosuppression.
Methods: Our infectious disease team assesses patients 1 year post- heart and liver transplant to determine need to continue Pneumocystis jirovecii (PJP) prophylaxis. We reviewed flow cytometry results obtained at this visit based on clinical history and compared CD4 counts between patients. Liver transplant patients did not receive induction immunosuppression. Heart transplant patients received thymoglobulin as induction. Many patients with CD4 count < 500 at one year post-transplant had repeat flow cytometry 3 months later.
Results: 11 liver and 22 heart transplant recipients were included. Eight patients had repeat flow cytometry. 7 patients had CD4 <200, 10 had CD4 200-500, and 16 had CD4 >500. Liver transplant recipients were unlikely to have low CD4 counts 1 year post-transplant (9% CD4 200-500). Patients with congenital heart disease, especially with a history of single ventricle physiology, had frequent low CD4 counts, which almost always stayed low when rechecked 3 months later. Only 2/8 patients with repeat flow cytometry had improvement to the next group (<200 to 200-500 or 200-500 to >500); both had heart transplants for cardiomyopathy. The other 6 had persistently low CD4; all were transplanted for SV physiology.
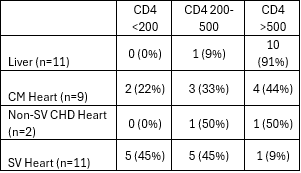
Discussion: This small study found that while most pediatric liver and non-CHD heart transplant patients have normal CD4 counts at a year post-transplant, patients with CHD and particularly, SV physiology, are much more likely to have persistently low CD4 counts a year post-transplant. While there are few patients who have yet had repeat flow cytometry after the one-year mark, those who had SV physiology were unlikely to recover CD4 counts in subsequent months.
These findings may be related to early palliative cardiac surgery and partial thymectomy. It raises concern that patients with SV physiology should be treated differently from other patients when considering induction and maintenance immunosuppression. Routine flow cytometry to assess PJP risk post-transplant is warranted, especially in heart transplant patients. Further evaluation is needed to understand the natural history of the immune system after transplant in a wide variety of pediatric patients to understand the natural history of the immune system’s response to the level of immunosuppression received. This might eventually allow enough understanding to tailor immunosuppression to minimize risks of infection and rejection.
[1] Immunosuppression
[2] Flow Cytometry
[3] CD4 Count
[4] Heart transplant
[5] Liver transplant
[6] Thymoglobulin
[7] Single ventricle physiology