Liver transplantation in metabolic diseases: A 17-years single center experience
Silvio Veraldi1, Gionata Spagnoletti2, Luca Della Volpe1, Daniela Liccardo1, Maria Sole Basso1, Alberto Maria Fratti2, Riccardo Cirelli2, Marta Maistri2, Simone Reali3, Mariangela Padua3, Paola Francalanci4, Lidia Monti5, Gianluigi Natali6, Diego Martinelli1, Roberta Taurisano1, Barbara Siri1, Arianna Maiorana1, Andrea Pietrobattista1, Carlo Dionisi Vici1, Marco Spada2.
1Division of Metabolic diseases and Hepatology, Bambino Gesù Children's Hospital, IRCCS, Rome, Italy; 2Division of Hepatobiliopancreatic Surgery, Liver and Kidney Transplantation, Bambino Gesù Children's Hospital, IRCCS, Rome, Italy; 3Division of Anesthesiology and Critical Care, Bambino Gesù Children's Hospital, IRCCS, Rome, Italy; 4Division of Pathology, Bambino Gesù Children's Hospital, IRCCS, Rome, Italy; 5Division of Gastrointestinal Imaging and Liver Transplantation, Bambino Gesù Children's Hospital, IRCCS, Rome, Italy; 6Interventional Radiology Unit, Bambino Gesù Children's Hospital, IRCCS, Rome, Italy
Introduction: Metabolic diseases (MD) represent the second most common indication for liver transplantation (LT) in children. Indications include prevention of metabolic decompensation, treatment of the liver disease and improvement of neurological outcomes and organ damage.
Methods: We retrospectively reviewed the clinical records of patients who underwent LT for MD at the Bambino Gesù Children’s Hospital from January 2008 to February 2025.
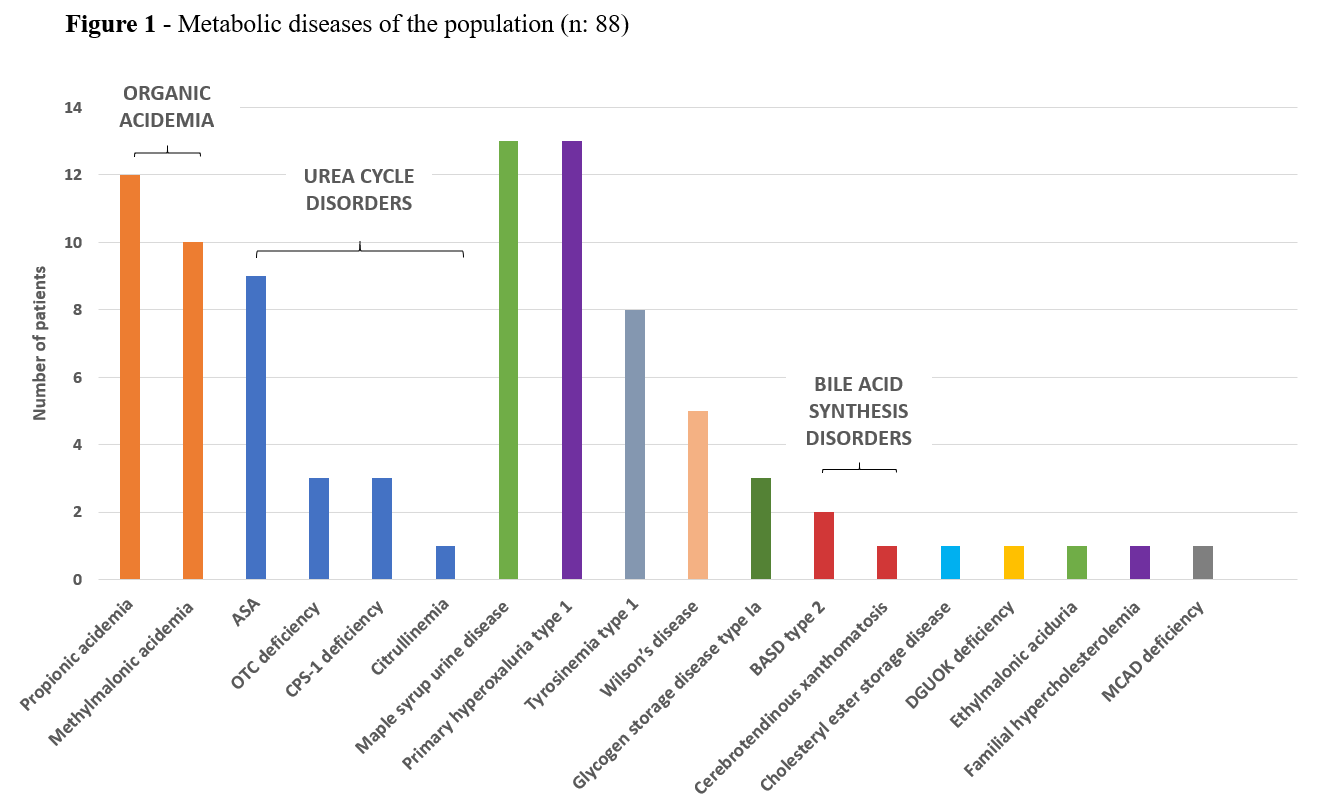
Results: 88 out of 395 (22.3 %) (age: 90.5 months, IQR: 72) children underwent a LT for MD. Weight and height z-score were -0.855 (IQR: 2.2) and -0.887 (IQR: 2.45). 18 had a MD with structural liver disease (ALF, HCC or ESLD) with a median MELD/PELD of 28 (IQR: 15): tyrosinemia type 1 [n:8, 8.8%], Wilson’s disease [n: 5, 5.7%], bile acid synthesis disorders [n: 3, 3.4%], DGUOK deficiency and cholesteryl ester storage disease [n: 1 (1.1%) for each]. 70 underwent LT without structural severe liver disease: organic acidemias [n: 22, 25%], urea cycle disorders [n: 16, 18.2%], maple syrup urine disease [n: 13, 14.8%], primary hyperoxaluria type 1 [n: 13, 14.8%], glycogen storage disease type Ia [n: 3, 3.4%], others [n: 3 (3.3%)] (Fig. 1). Heterozygous living donor LTs were performed in 16 (18.2%); deceased donor whole and split livers transplantation in 25 (28.4%) and 47 (53.4%). 8 had a combined or sequential liver-kidney transplant. A patient with MSUD who underwent LT provided a whole liver for a child with biliary cirrhosis. After 63.9 months (IQR: 72) (median follow-up) patient and graft survivals were 96.6% and 94.4%: 2 died because of perioperative complications, 1 of cardiorespiratory failure with normal liver function. 2 pts were retx because of EGD. In the 1-year after LT, 8 (9%) required relaparotomy; 6 (7%) and 13 (15%) developed vascular and biliary complications successfully treated with interventional radiology and/or endoscopy. 27 had an acute liver rejection (30.7%). Sepsis/bacteriemia were reported in 19 (21.6%). CMV viremia was seen in 41 (46.6%) with pre-emptive treatment needed in 21 (23.9%). EBV viremia was reported in 60 (68.2%) with 45 already positive before LT. Throughout the follow-up period, 4 patients (4.5%) were diagnosed with PTLD/lymphoma. 14 (15.9%) experienced either acute or chronic neurological complications (i.e. PRESS, seizures, or tremors) with 4 attributed to CNI toxicity. With the exception of one patient (propionic acidemia), no metabolic decompensation was observed after LT. All children resumed a normal protein intake within 4 weeks. 1-year after LT, patients presented a median increase in height and weight z-scores of 0.389 (IQR: 2.15) and 0.181 (IQR: 1.74).
Conclusion: LT in MD had excellent outcomes with a significant regression of the risk of metabolic decompensation and an improvement in QoL. Long-term data are needed to evaluate the role on neurological and organ damage. Close follow-up and timely transplantation are key factors in the management of these patients.
[1] Liver transplant
[2] Metabolic diseases