Strategies for improving influenza vaccination rates in pediatric transplant recipients
Lindsey Shinn1, Patricia Fredrick1, Elizabeth Eliopoulos1, Kristin Rich1, Hannah Foiles1, Alicia House1, Nancy Koenig1, Vikas Dharnidharka2, Raja Dandamudi2, Janis Stoll3, Sakil Kulkarni3.
1Transplant Services, St. Louis Children's Hospital , St. Louis, MO, United States; 2Department of Nephrology, Washington University St. Louis, St. Louis, MO, United States; 3Department of Hepatology , Washington University St. Louis, St. Louis, MO, United States
Pediatric solid organ transplant recipients are at a higher risk for vaccine-preventable infections than the general population. A recent multicenter study demonstrated a hospitalization rate of up to 87 times higher for pediatric liver transplant recipients in the first 5 years of follow-up (Feldman et al., 2019). In 2021, the St. Louis Children’s Hospital (SLCH) Abdominal Transplant Program observed lower influenza vaccination rates than in previous years. Given the higher risk of infection in the immunocompromised population, and the surge in hospital admissions for COVID-19 and respiratory syncytial virus, the team elected to initiate a quality improvement project for 2022 in hopes of standardizing the approach to vaccination.
The team utilized the Plan-Do-Study-Act (PDSA) method to identify barriers, plan for improvement, and optimize outcomes. The aim was to achieve a >90% influenza vaccination rate in each organ group by 12/31/2022. To accurately collect the data, a Tableau dashboard was created which included the total number of eligible patients, the number of vaccinated patients, and the percentage of vaccinated patients. The report also pulled in the names of patients who had not been vaccinated. To achieve reliable results, the team created a standardized approach to project management. The manager distributed weekly emails to all team members regarding the team’s progress. The emails also included the names of the patients who had not received the vaccination. For any patient who had not received the vaccine, the nurse was asked to discuss the vaccine with the family on a follow-up phone call. The physician and nurse also added the discussion topic to their clinic workflow. With the frequently scheduled clinic visits for this population and the ability to administer the vaccine in the clinic, access became an important factor in the success of the project.
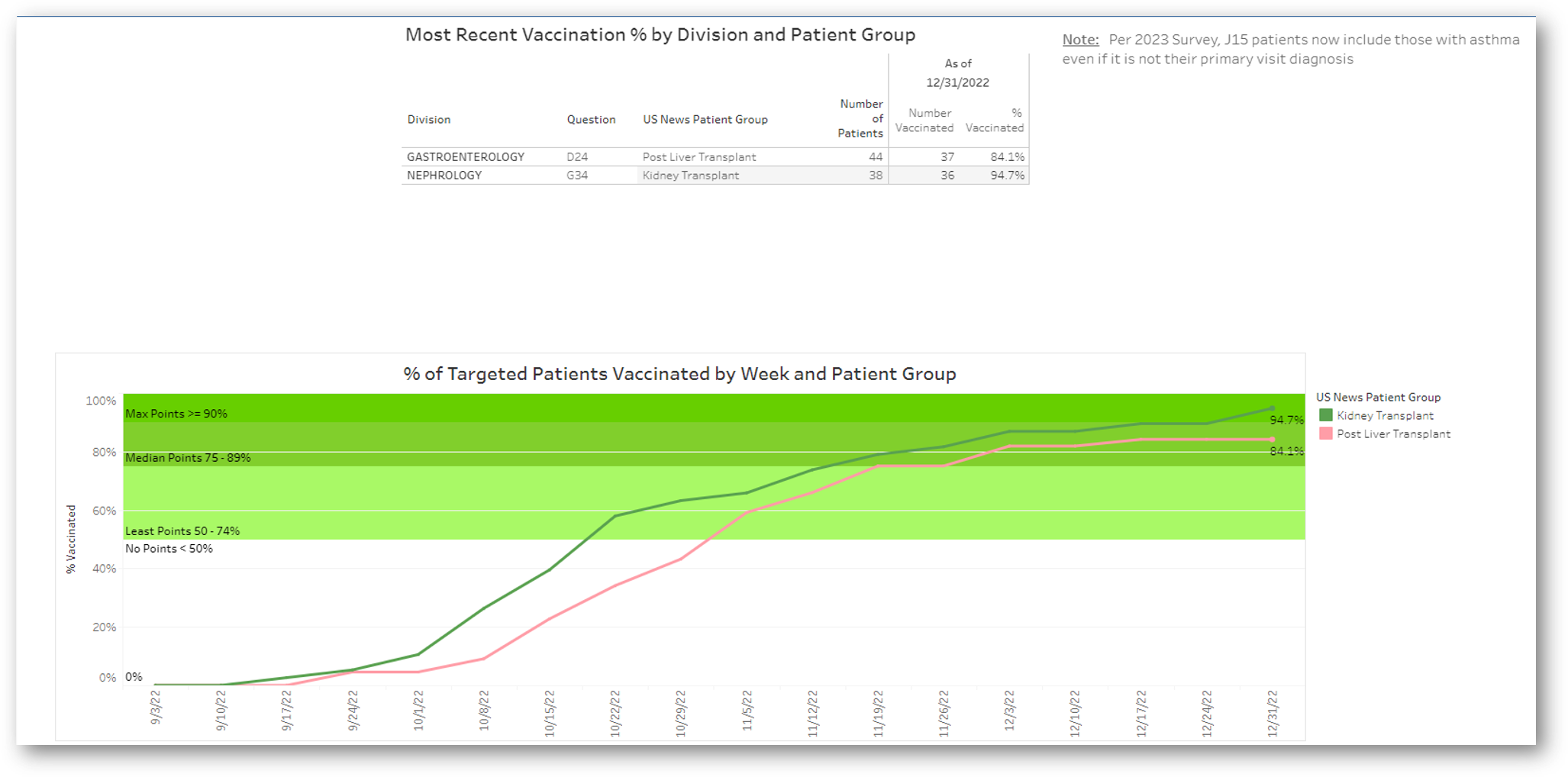
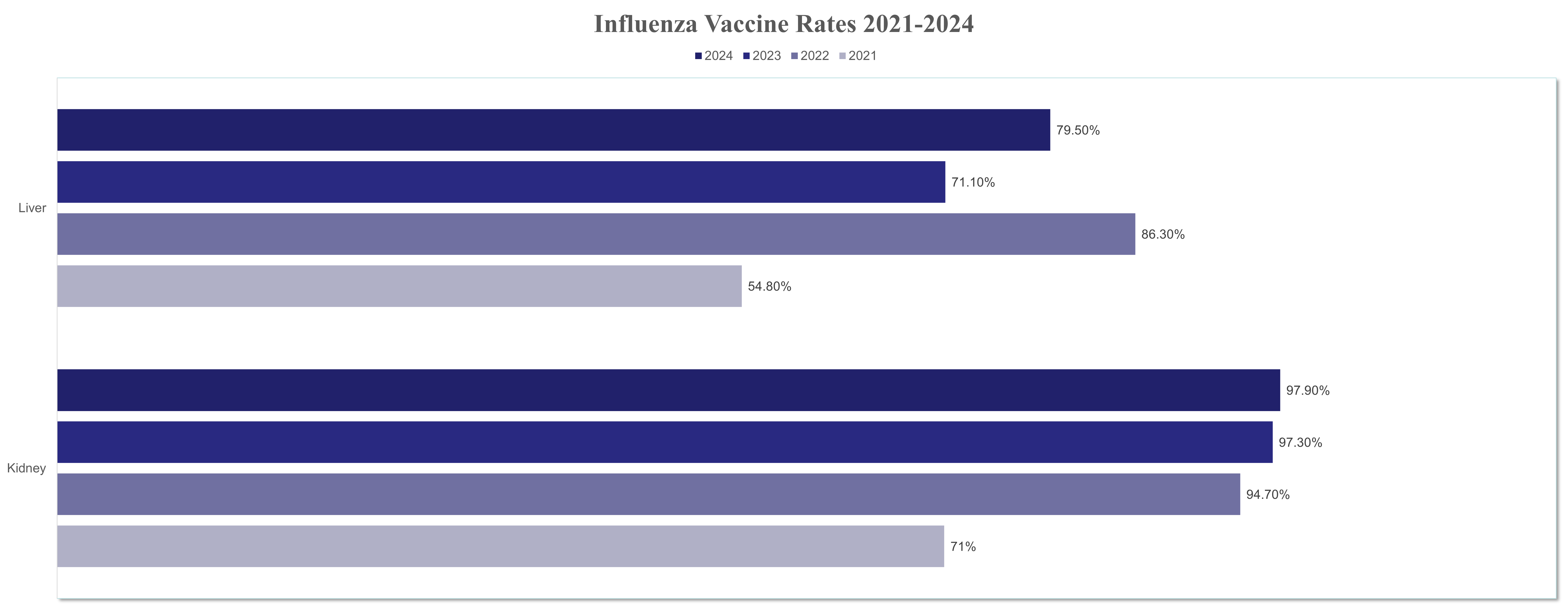
Data was collected on eligible patients who were seen by the program between October 1 and December 31, 2022. The overall rate for post-kidney transplant recipients in 2021 was 71%. After implementation, the the team was able to vaccinate 36 out of the 38 eligible patients, achieving a 94.7% vaccination rate. Although the liver transplant team did not achieve a >90% vaccination rate, they demonstrated a more significant improvement in overall numbers. The overall rate for post-liver transplant recipients in 2021 was 54.8%, but the team was able to vaccinate 38 out of 44 eligible patients, achieving an 86.3% influenza vaccination rate. Both teams have been able to sustain increased numbers through 2024 after successfully completing multiple PDSA cycles, with the addition of Infectious Disease consults and 100% utilization of the Pre-Visit Planning Tool.
Standardization, frequent communication, and accessibility are effective methods for improving vaccination rates in the pediatric post-transplant population.
[1] Influenza
[2] Vaccinations