The spectrum of post-transplant diabetes mellitus in children in a tertiary care hospital in India
Indira Agarwal1, Lakhmee Naorem 1, Deepthi R V1, Georgie Mathew1, Rouba Garro2.
1Pediatric Nephrology, Christian Medical College, Vellore, India; 2Pediatric Nephrology, Children’s Healthcare of Atlanta and Emory School of Medicine,, Atlanta, GA, United States
Introduction: PTDM occurs in 3–20% of pediatric transplant patients depending upon the organ transplanted, age at transplantation, immunosuppressive regimen administered, family history of metabolic syndrome and diabetes, and lifestyle factors.
Methodology: A single-center, retrospective study was conducted on children less than 18 years of age who received kidney transplants (KT) between November 2017 and June 2023. Evaluation for developing hyperglycemia and diabetes post-transplant (PTDM) was performed.
The demographic profile, medication administered, duration and severity of hyperglycemia, treatment given, and outcome were compared with children who did not develop PTDM. Statistical analysis was done using SPSS. Continuous data were expressed as means and standard deviations (SD), categorical data as numbers and percentages, p < 0.05 was considered statistically significant.
Results: Of the 18 KT recipients, 4 patients developed PTDM (22%). Mean age at ESKD was 11.75 ± 1.7 years; mean age at transplantation was 12.63 ± 1.7 years. The underlying kidney disease was CAKUT in 75%, 25% had chronic glomerulonephritis. Majority were male (3/4). At 3 months, mean weight gain in PTDM group was 8.2 ± 2.2 kg as against 6.9+/-1.5 in the non PTDM group (p=0.097). BMI gain was 3.2 kg/m post-transplant with a p-value of 0.074. One of the parents was diabetic in 50% of patients with PDTM.
Median duration of onset of hyperglycemia was 32 days (IQR-9-70 days). Management of hyperglycemia varied from modification of immunosuppressive medications to use of anti-hyperglycemic agents. Insulin therapy was required in 50% (2/4) for a mean duration of 53 days (range 50-55 days). Mean steroid dose at onset of PTDM was 13.75 ± 7.2mg. One patient had acute tacrolimus toxicity with trough level (C0) of 13.2ng/ml and an average level of 8 ng/mL (2.8, 13). Mean serum magnesium level at one-month was 1.28 ± 0.5 mg/ml in the PTDM group compared to (1.9±0.2 mg/dl) in the non-PTDM group (p= 0.061).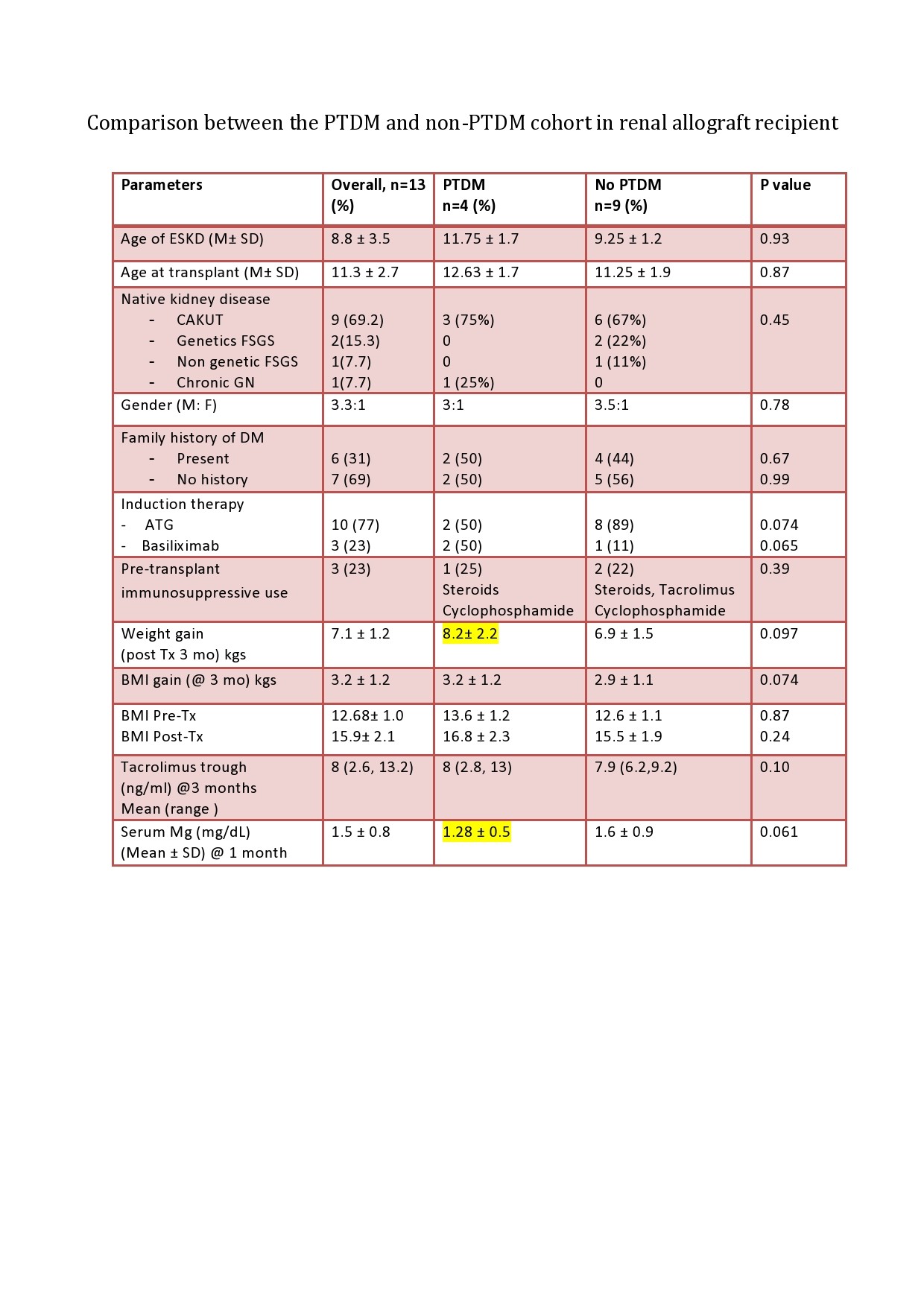
All children had resolution of hyperglycemia after appropriate intervention and management of hyperglycemia. Mean time to hyperglycemia resolution was 252 ± 56 days. There were no acute rejection episodes but 50% of the children had acute kidney injury which resolved after resolution of hyperglycemia.
Conclusion: PTDM is a well-recognized metabolic complication of pediatric KT. Awareness of risk factors and regular monitoring facilitate the timely detection of hyperglycemia. Early intervention and lifestyle modification are associated with good outcomes and complete reversal of PTDM and hyperglycemic state.
[1] PTDM
[2] hyperglycemia
[3] Children