Bridging the gap: Navigating donor-recipient size mismatch in pediatric renal transplants
Ahmad Azzam1, Mansour Tawfik1, Heba BAhbah1, Mahmoud Obeid1, Al Anoud Al Shami1.
1Multi Organ Transplant Center, King Fahad Specialist Hospital, Dammam, Saudi Arabia
Background: Size mismatch between Donor and recipient usually occurs in pediatric kidney transplantation (KT). No clear studies for its effect on graft function and survival. We aimed to highlight the effect size mismatch between donor and recipients on the immediate, long-term survival and function of transplant kidneys in pediatric . We used the BSAi (Donor body surface area /Recipient body surface area) to study whether transplanting a relatively small or large kidney in pediatric relative recipient will impact on different renal transplant outcomes.
Patients and Methods: This retrospective study investigated the impact of donor-recipient size mismatch, quantified by body surface area ratio (BSAi), on graft outcomes in 210 pediatric kidney transplant recipients. The cohort was categorized into four BSAi groups: BSAi <1 (recipient larger than donor), BSAi 1-<2, BSAi 2-<3, and BSAi ≥3 (donor progressively larger than recipient). The majority of donors were adults, highlighting the prevalence of size mismatches in pediatric kidney transplantation.
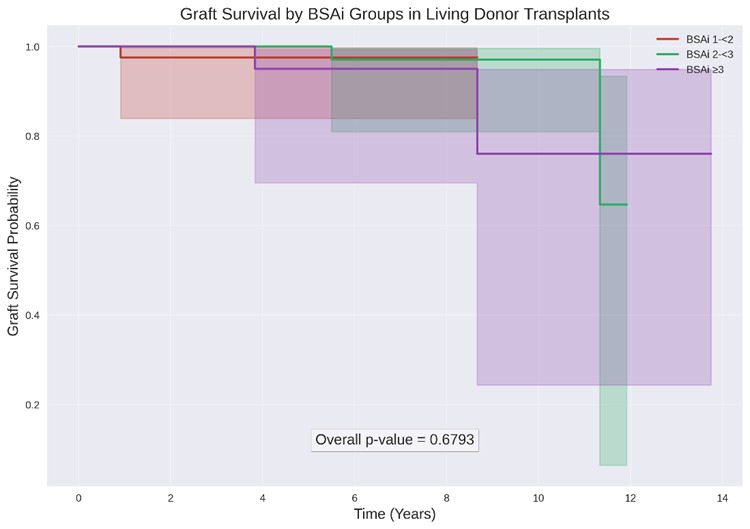
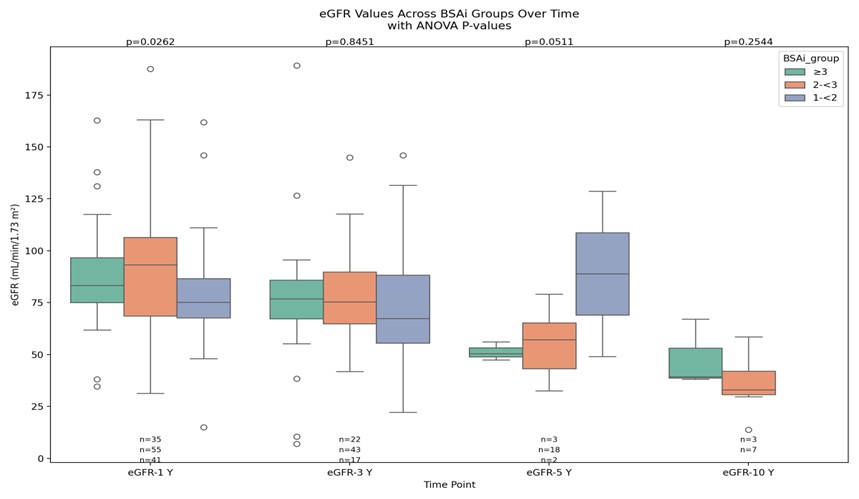
Results: The study found no significant association between BSAi categorization and immediate graft outcomes, delayed graft function (DGF), or graft survival in both living and deceased donor transplants. However, the limited number of graft failure events and abbreviated follow-up period necessitate larger cohort studies to validate these findings. In living donor transplants, BSAi-associated differences in renal function were most pronounced early post-transplant but tended to equilibrate over time. For deceased donor transplants, BSAi significantly influenced medium-term graft function at 3 years, with BSAi <1 recipients experiencing superior renal function, but this benefit attenuated over time.
Conclusion: The study suggests that donor-recipient size mismatch may no longer significantly compromise neither immediate nor long-term graft survival in pediatric kidney transplantation under optimum medical and surgical settings. The findings open up possibilities for potentially bolder and more secure pediatric kidney transplantation strategies in the future.