Is there a difference in outcome between DCD and DBD donor kidneys in pediatric transplant recipients? A nationwide analysis
Huib De Jong1, Femke Vrieling-Prince1, Mandy Keijzer-Veen2, Charlotte Bootsma-Robroeks3, Antonia Bouts4, Marlies Cornelissen5.
1Pediatric Nephrology, Erasmus MC Transplant Institute, Rott, Netherlands; 2Pediatric Nephrology, University Medical Center Utrecht, Utrecht, Netherlands; 3Pediatric Nephrology, University Medical Center Groningen, Groningen, Netherlands; 4Pediatric Nephrology, Amsterdam UMC, Amsterdam, Netherlands; 5Pediatric Nephrology, Radboud UMC, Nijmegen, Netherlands
Kidnie consortium.
Aims/Purpose: Although pre-emptive living kidney donation is the first-choice treatment modality for pediatric patients with end stage renal disease in the Netherlands, we still have the need for a post-mortal kidney donor program. Despite the fact that brain dead heart beating donors (DBD) are scarce, we are cautious to use non-heart beating donors after circulartory death (DCD) because of the risk for delayed graft function and reduced graft survival. Since 2000 the DCD program has evolved from static cold storage of the kidney (‘kidney on ice’, similar to the DBD protocol) towards a successfull nation wide machine perfusion protocol.
We questioned whether our cautiousness to use DCD donors is still justified and aimed to evaluate the outcome of DCD kidneys compared to DBD and living donor kidneys in pediatric recipients.
Methods: All children who received a kidney graft between 2012 till 2024 were included. The recipients were analysed based on the donor type (living-, DBD- or DCD donor). Graft recovery in the first week after transplantation and at 3 months as well as graft survival and dialysis waiting time were evaluated.
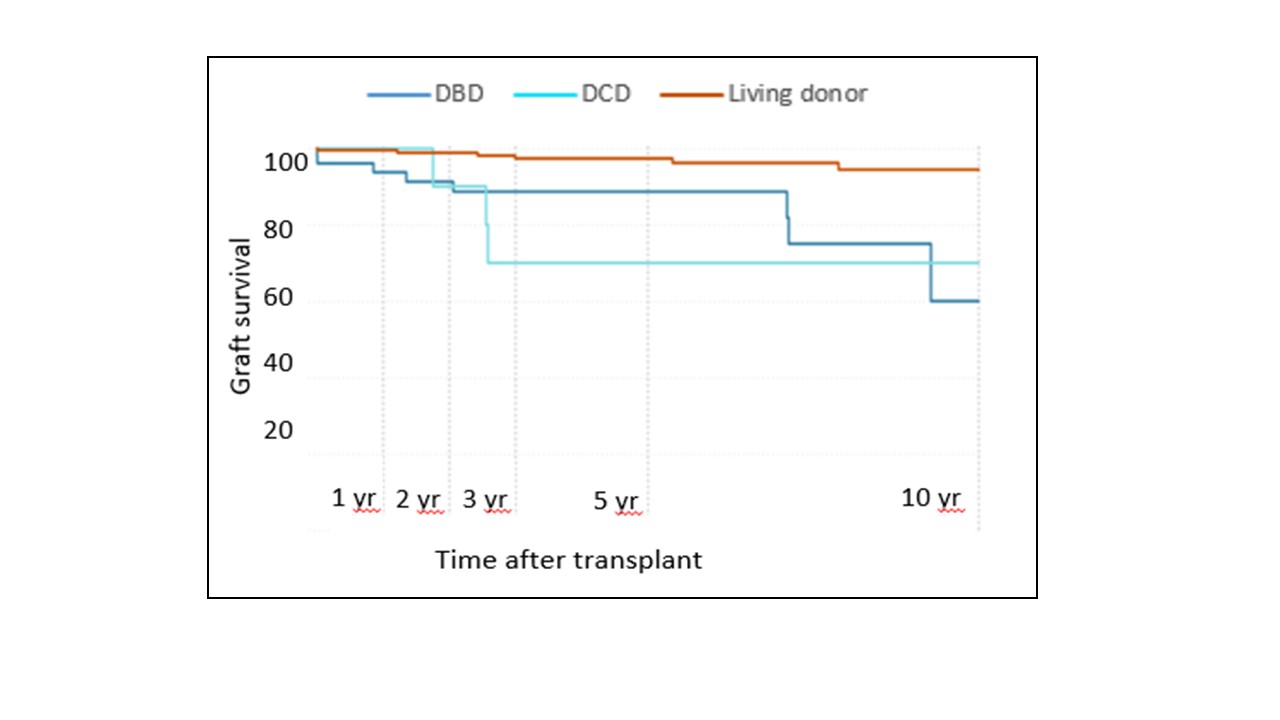
Results: In total 261 pediatric recipients received a kidney transplantation. Of them 192 (74%) received a living donor and 69 (26%) a post mortal donor. Of the 69 post-mortal donors, 15 (22%) were of DCD origin while 54 (78%) were from a DBD donor. Graft recovery of the living donor kidneys was superior to the DBD group which was again superior to the DCD group. Nevertheless at 3 months post transplantation the kidney function was similar irrespective of the organ type used. The 10 year graft survival was for living-, DBD and DCD donors respectivity 94%, 60% and 70%. (P=<0,05) Thus, a significant graft survival benefit when using a living donor, but no difference in graft survival between DBD and DCD donors. Importantly, we saw that by implementing the different kidney transplantation programs we were able to lower the dialysis waiting time for an organ from 3 years to less then 1 year at the moment.
Conclusion: Although a slower graft recovery the outcome of DCD kidneys is similar to DBD kidneys and therefore these organs can safely be used in pediatric recipients who don’t have the opportunity for living donation. In the Netherlands this program (togheter with other programs) has resulted in a substantial decline in dialysis waiting time.
[1] allograft survival
[2] donation after circulatory death
[3] donation after brain death