
Professor Stephen Marks, MD MSc MRCP DCH FRCPCH is Professor of Paediatric Nephrology and Transplantation at University College London Great Ormond Street Institute of Child Health and President of the British Association for Paediatric Nephrology. He is clinical lead for renal transplantation and Director of the National Institute for Health Research Great Ormond Street Hospital Clinical Research Facility at Great Ormond Street Hospital for Children NHS Foundation Trust. He has local, national and international roles including Chair of the Education Committee of the International Pediatric Transplant Association (IPTA) having also been an IPTA Councillor. His research continues to date in the fields of renal transplantation (including innovative drug trials concerning new anti-rejection therapies and assessment of children post-renal transplantation), systemic lupus erythematosus and vasculitis. He is on the editorial board for “Pediatric Nephrology” and “British Journal of Renal Medicine” and is associate editor for “Transplantation” and “Pediatric Transplantation”, which are the journals of The Transplantation Society (TTS) and the International Pediatric Transplant Association (IPTA), respectively.
Transition processes for adolescent kidney transplant recipients to adult care
Hai Liang Tan1,2, Claire Gaymer1, Jong Eun Song1, Stephen D Marks1.
1Paediatric Nephrology, Great Ormond Street Hospital, London, United Kingdom; 2Paediatric Nephrology, Women and Children Hospital Kuala Lumpur, Kuala Lumpur, Malaysia
Aims/Purpose: Adolescents have reduced renal allograft survival rates due to reduced adherence to medications and changing immune system, especially when there has been little or no transition to young adult kidney transplant services. NICE has published guidance in the United Kingdom, that outlines quality statements for an effective transition programme. In addition, effective transition must meet the needs of today’s increasingly complex patients. Complex patients include those with multiple care needs who are served by multiple providers, have several co-morbidities, come from disadvantaged socioeconomic backgrounds and/or have learning difficulties or behavioural traits that present challenges in caring for them. The primary aim of this study was to describe the cohort of kidney transplant recipients who transition from a paediatric tertiary centre. The secondary aim of this study is to describe the transition process that they underwent.
Methods: Retrospective, single-centre study of all kidney transplant recipients who transferred to adult services from January 2022 to April 2024. Data regarding baseline characteristics, transition process and complexity were collected.
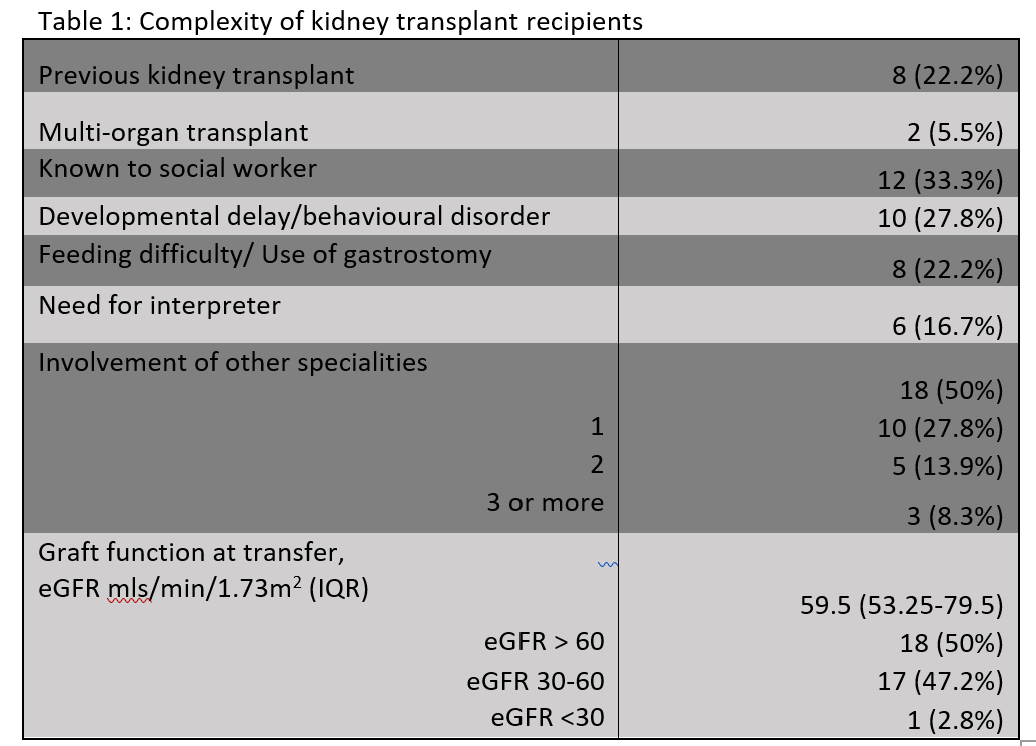
Results: Thirty six (53% male; 56% living donor) adolescent kidney transplant recipients with a functioning graft commenced transition at median age of 16.0 years and whose care was transferred to adult services. More than half of the patients (56%) received their transplant before the age of 13 years. The most common primary kidney disease was CAKUT (50%). Most patients (77.8%) had a period of dialysis prior to transplant and the median time from transplantation was 6.0 (1.5 - 10.5) years. Most patients were complex and had involvement of other specialities as well as multiple needs. (Table 1)
All patients from our centre had annual meetings to review transition planning and a named worker to coordinate care. However, one quarter of patients did not have a named worker in the adult receiving centre. Two thirds of patients attended joint clinic with adult practitioner before transfer while 83.3% had a clinic review prior to transfer.
Conclusions: This study highlights the changing landscape of transition where there is a growing population of complex adolescent kidney transplant recipients whose care is being transferred to adult services. This reflects the improving survival of patients who may not
previously have been candidates for kidney transplantation. There is an urgent need to improve transition programmes to cater to the additional needs of complex patients with improved education on medical complexity and providing support for patients and their families.
[1] Adolescent
[2] Young adult
[3] Kidney transplantation
[4] Transfer
[5] Transition to adult care.