Changes in plasma citrulline after liver transplantation in patients with inborn errors of metabolism: Non-invasive recovery indicator of intestinal function?
Luca della Volpe 1, Daniela Liccardo 1, Silvio Veraldi1, Maria Sole Basso1, Roberta Taurisano1, Sara Cairoli1, Alberto Maria Fratti2, Gionata Spagnoletti2, Riccardo Cirelli2, Marta Maistri2, Fabrizio Chiusolo3, Rosanna Pariante3, Paola Francalanci4, Lidia Monti5, Giovanna Soglia5, Diego Martinelli1, Andrea Pietrobattista 1, Marco Spada2, Carlo Dionisi Vici1.
1Division of Metabolic diseases and Hepatology, Bambino Gesù Children's Hospital. ERN TransplantChild, MetabERN, RareLiver., Rome, Italy; 2Division of Hepatobiliopancreatic Surgery, Liver and Kidney Transplantation, Bambino Gesù Children's Hospital. ERN TansplantChild, RareLiver., Rome, Italy; 3Division of Anesthesiology and Critical Care, Bambino Gesù Children's Hospital, Rome, Italy; 4Division of Pathology, Bambino Gesù Children's Hospital, Rome, Italy; 5Division of Gastrointestinal Imaging and Liver Transplantation, Bambino Gesù Children's Hospital, Rome, Italy
Introduction: liver transplantation (LT) is a rising treatment option in several Inherited Metabolic Diseases (IMD). Plasma citrulline, a non-protein amino acid synthesized by small bowel enterocytes, has been explored as a potential biomarker of intestinal function and enterocyte mass. The study aims to determine whether citrulline levels could represent an indicator of intestinal function’s after LT.
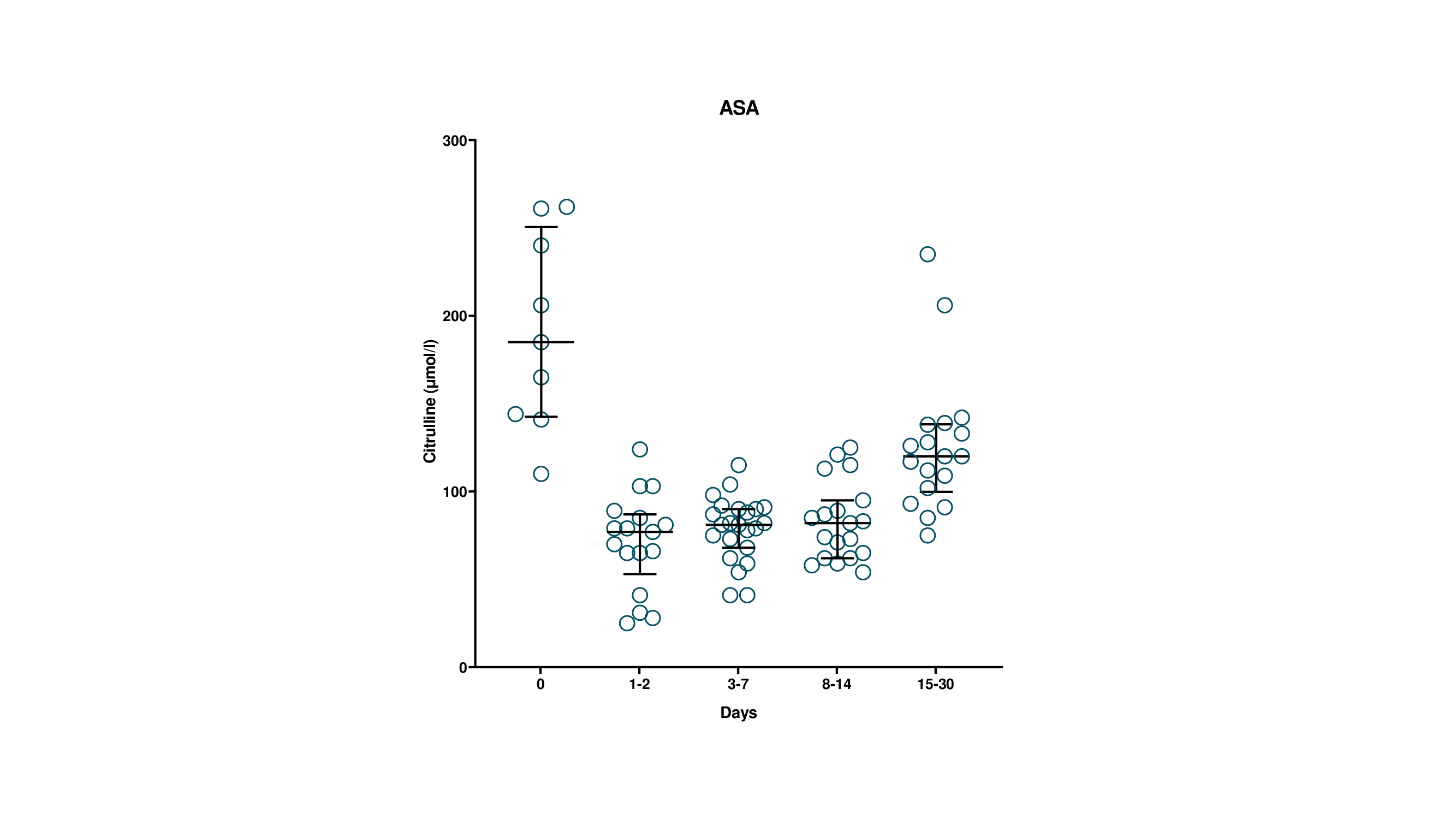
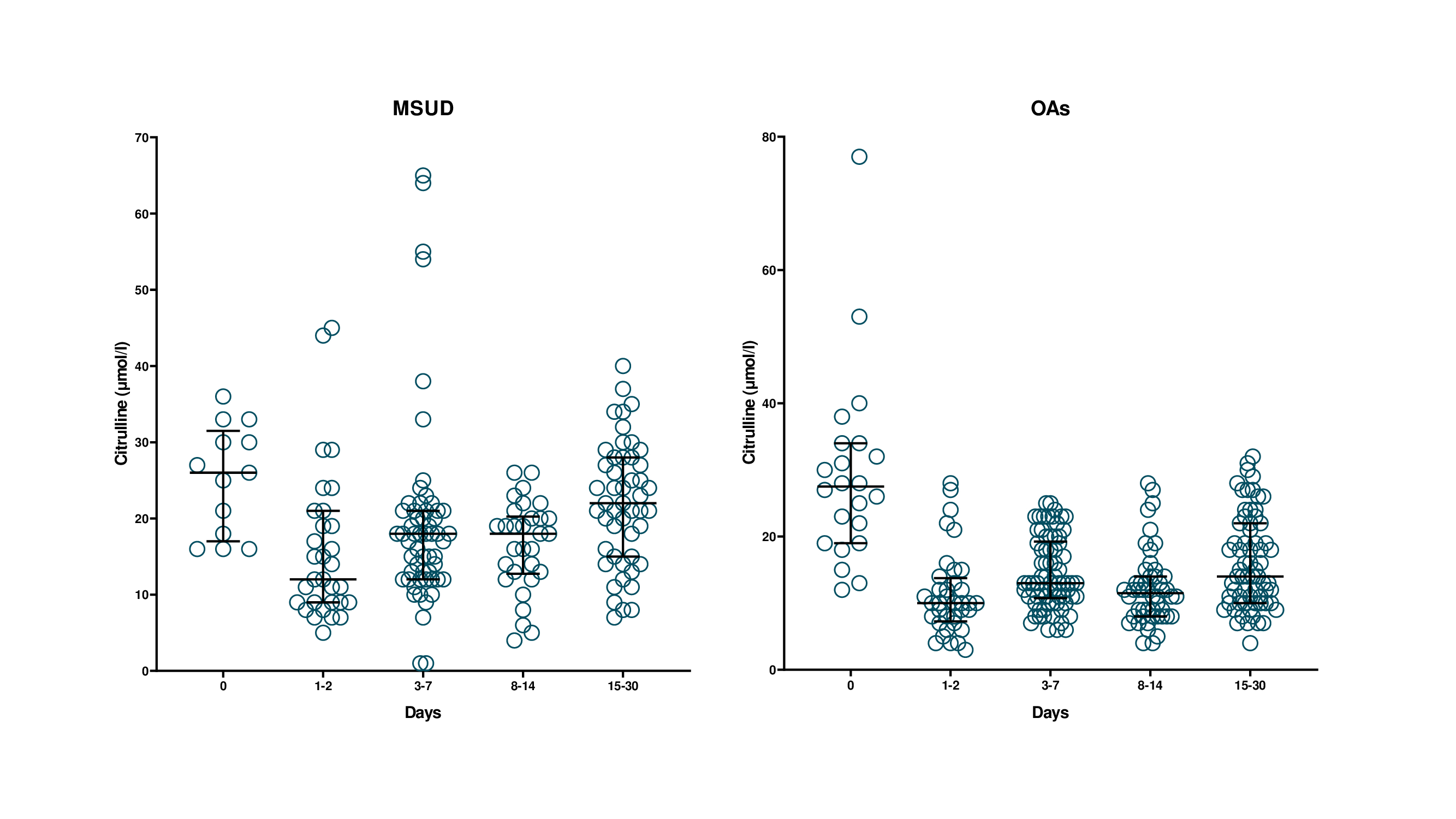
Methods: 44 IMD patients who underwent LT from 2013 to 2024 were retrospectively included in the study. As a standard protocol, plasma aminoacid levels (including citrulline) were systematically analyzed after LT at different points (LT, 1-2, 3-7, 8-14, 15-30 post-operative days). Patients were divided in three diagnostic groups Argininosuccinic Aciduria (ASA, 9 pts), Organic Aciduria [OAs (MMA & PA), 22 pts], and Maple Syrup Urine Disease (MSUD, 13 pts).
Results: Prior to LT, citrulline levels were in the expected ranges for the specific metabolic defect. After LT, citrulline levels sharply declined within the first 48 hours, followed by a progressive raise to pre-LT values within the first 4 weeks post-LT (p < 0.05). As expected, ASA patients exhibited significantly higher citrulline levels at any study time compared to other IMD groups (p < 0.05). In ASA patients, the median plasma citrulline at LT was 185 μmol/l (144-240), falling to 77 μmol/l (65-85) in the first two days after LT, and then returning to 120 μmol/l (104-137) one month after LT. Patients with MSUD and OAs showed normal median citrulline levels prior to LT [26 μmol/l (18-30) and 28 μmol/l (20-34), respectively] with a rapid reduction immediately after LT [12 μmol/l (9-20) and 10 μmol/l (8-13), respectively], followed by a return to pre-LT levels after one month in MSUD [22 μmol/l (15-28)], with a less pronounced rise in OAs [14 μmol/l (10-22)]. Higher early post-LT citrulline levels correlated with a shorter duration of parenteral nutrition (p <0.05). Resumption of bowel movements occurred at a median time of 5.5 days post-LT, which corresponded to a rise in plasma citrulline levels. None of the patients had surgical or medical intestinal complications.
Conclusions: The study showed that, regardless of the disease category, plasma citrulline levels present an early reduction after LT, followed a progressive increase once resuming bowel movements, thus providing the proof of principle that longitudinal monitoring of plasma citrulline may represent a non-invasive marker of post-LT enterocyte function.
[1] Liver Transplantation
[2] Inborn Metabolic Disease
[3] Citrulline