Pediatric ACLF, optimizing outcomes through timely living donor liver transplantation
Muhammad Amar Qudeer1, Muhammad Yasir Khan1, Sohail Rashid1, Ihsan UL Haq1, Faisal Saud Dar1.
1HPB and Liver transplant, Pakistan kidney and Liver institute and research center, Lahore, Pakistan
Introduction: Liver transplantation remains the definitive treatment option for acute-on-chronic liver failure (ACLF), despite advancements in medical management. Living donor liver transplantation (LDLT) has become a critical option, particularly in pediatric cases, given the limited availability of deceased donor organs. As there is no consensus on pediatric acute-on-chronic liver failure (ACLF), it is defined as the acute deterioration of pre-existing compensated or decompensated cirrhosis, usually related to a precipitating event, which can be hepatic or systemic. This study aims to analyze the optimal timing and outcomes of pediatric LDLT for ACLF, focusing on timing, patient demographics, clinical scores, donor variables, prioritizing early graft availability for transplantation, and post-transplant complications.
Methods: A retrospective analysis using a prospectively maintained database was conducted on patients who underwent LDLT for ACLF from January 2024 to March 2025 at a specialized transplant center. Data were obtained from electronic health records, including demographic details, full clinical data, liver-specific assessments (CTP), donor characteristics, graft details, surgical outcomes, and post-transplant complications. Statistical tests (Independent Samples t-test, Mann-Whitney U) were performed to compare operative outcomes (e.g., surgery duration, blood loss) between patients. Linear regression models were used to assess the impact of time to transplant on outcome variables.
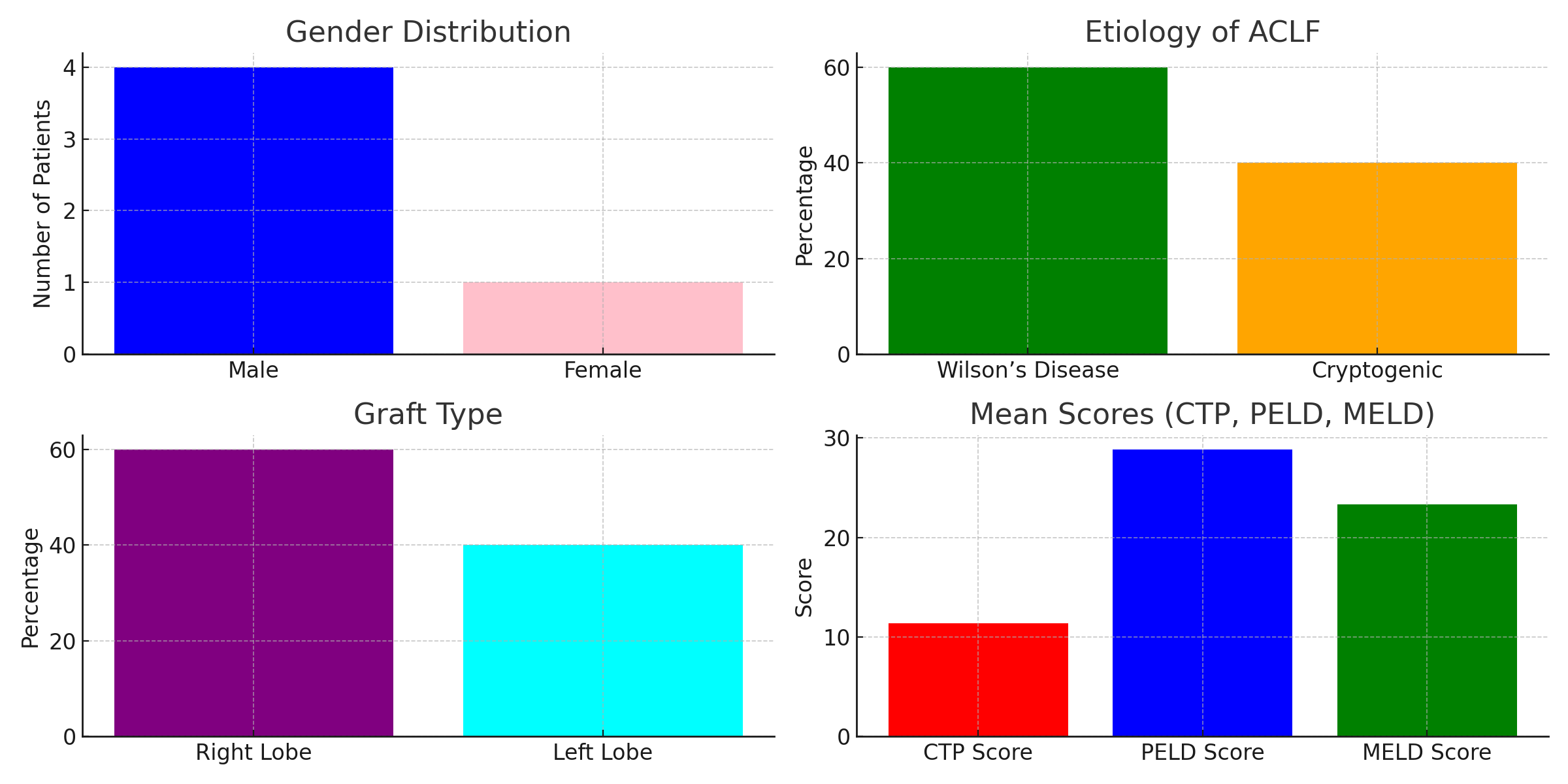
Results: Data from five patients presenting with ACLF were analyzed. Four patients were male (80%), and one was female (20%). The patients' ages ranged from 1 to 15 years, with a mean age of 8.8 years; the youngest patient was 1 year old, and the oldest was 15 years old. The most common etiology of ACLF was Wilson’s disease (60%), followed by cryptogenic causes (40%). The mean CTP score was 11.4, the mean PELD score was 28.85, and the mean MELD score was 23.33, indicating severe liver disease. The time to transplant ranged from 48 to 72 hours for all cases, except one case that took 23 days for optimization. Graft types included 60% right lobe and 40% left lobe grafts, with a mean graft-to-recipient weight ratio (GRWR) of 1.45. Surgical outcomes were favorable, with minimal blood loss and transfusion requirements. Post-transplant patient survival was 100%, with no reported 30-day mortality or major complications.
Conclusion: Pediatric LDLT for ACLF is a life-saving intervention with excellent outcomes when performed in a timely manner. Early recognition of ACLF, appropriate donor selection, meticulous surgical planning, and early organ availability and allocation in both living donor liver transplantation (LDLT) and deceased donor liver transplant settings are critical for success. Further studies are needed to establish standardized, unified definitions, prognostic scoring systems, and treatment protocols for pediatric ACLF.
[1] Pediatric Acute-on-chronic liver failure, pediatric liver transplantation, living donor liver transplant, Wilson’s disease, graft-to-recipient weight ratio, CTP score, PELD/MELD score.