Reducing time from outpatient dialysis initiation to transplant activation
Priyanka Chati1, Jessica Whittington1, Karissa Braden1, Priya Verghese1, Kaitlyn White1, Katrina Andracki1, Anne Bendelow1, Cara McGarry1, Stella Kilduff1, Ricardo Superina1, Mahima Keswani1.
1Pediatric Nephrology, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States
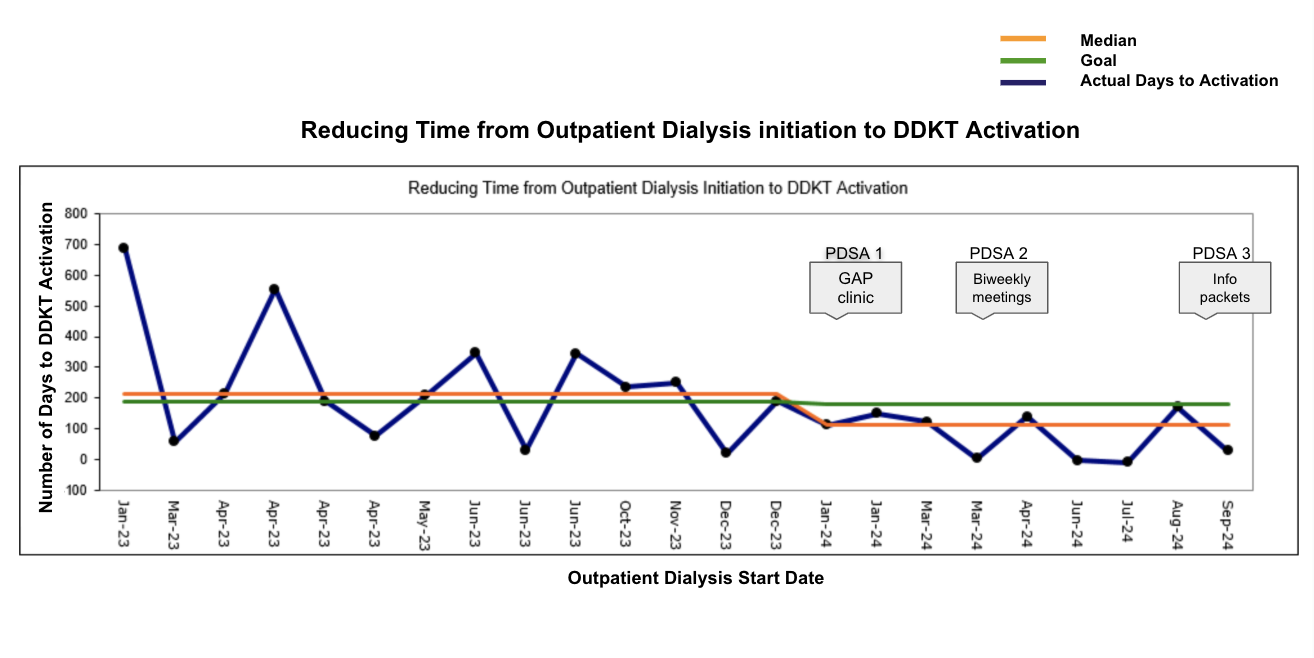
Introduction: Prolonged dialysis before transplantation increases mortality, morbidity, and reduces quality of life. While preemptive kidney transplantation is ideal, many patients require dialysis as a bridge. In 2023, 15 patients with end-stage kidney disease (ESKD) initiated dialysis (8 peritoneal, 7 hemodialysis) in our unit with a median time of 211.5 days to deceased donor kidney transplant (DDKT) activation. Our SMART aim was to reduce this median time by 10% to 190 days by the end of 2024.
Methods: Pediatric patients who started dialysis in 2024 and underwent DDKT evaluation were included. Exclusion criteria included patients under 1 year old and those with an active oncologic condition. Using a fishbone and driver diagram, key barriers were identified including communication gaps, limited patient knowledge, and cultural/social challenges. Three Plan-Do-Study-Act (PDSA) cycles were implemented to address these issues:
PDSA 1:Guidance and Planning (GAP) in Advanced Chronic Kidney Disease Clinic - Early education for advanced CKD patients and families on dialysis and transplantation before initiation
PDSA 2:Enhanced Communication Between Dialysis and Transplant Teams – Biweekly meetings between transplant coordinators and dialysis teams to review activation needs.
PDSA 3:Patient Education Materials – Distribution of an information booklet within the first week of dialysis initiation, covering CKD, transplant preparation, and a pre-transplant checklist.
Results: Among 15 dialysis patients, 5 were transplanted in 2023, 7 in 2024, and 1 in 2025, with 2 remaining on the list due to social/insurance barriers.
In 2024, 9 patients initiated dialysis (8 hemodialysis, 1 peritoneal dialysis). A run chart tracked progress after each PDSA cycle (Figure 1). The GAP clinic, launched in January 2024, held 15 sessions that year, improving patient preparedness. In March 2024, biweekly dialysis-transplant meetings began after hiring a second transplant coordinator in February 2024. This allowed dedicated oversight of chronic dialysis patients, facilitating timely clearance.
The final PDSA cycle focused on education. A bilingual information packet was introduced in September 2024 and received by 2 patients by year-end. The dialysis to activation time was decreased by 53%, achieving a median time of 112 days. Of the 9 patients starting dialysis in 2024, 6 (66.7%) were transplanted the same year, 2 (22.2%) in 2025, and 1 (11.1%) remains on the list as of February 2025.
Conclusion: By strengthening communication, enhancing targeted patient education, and identifying high-risk patients earlier, our initiative significantly reduced the time from dialysis initiation to transplant activation. This highlights the critical role of multidisciplinary collaboration and proactive patient engagement in optimizing transplant readiness. Future efforts should focus on maintaining these improvements and exploring additional strategies to further streamline the transplant evaluation process.
[1] Dialysis
[2] Transplant Activation
[3] Deceased Donor Transplant Activation
[4] Reducing Dialysis Time
[5] Transplant Activation Readiness
[6] Kidney Transplant