Model for multidisciplinary team activation at time of offer acceptance for liver transplant at LPCH
Danielle Romero-Iantorno1, Angela Wong1, Carmen Mandac1, Lauren North1, Katherine Harmann1, Alison Marshall1, Julie Depper1.
1Pediatric Liver Transplant, Lucile Packard Children's Hospital Stanford, Palo Alto, CA, United States
Introduction: For a patient and their family, the moment of an organ offer is the culmination of stressful days, weeks, or sometimes years of suffering from liver disease. For the transplant team, it is a time-sensitive process that requires collaboration across a spectrum of providers to prepare for major surgery along with the immediate postoperative period. Each case has variable requirements depending on the underlying diagnosis, comorbidities, and possible postoperative complications. We aim to describe our center’s transplant workflow, from the time of an organ offer to the transplant surgery, including a breakdown of the multidisciplinary roles and how they function within our standardized workflow. Our efficient model prioritizes patient and family-centered care, along with open channels of communication amongst the transplant team.
Methods: Attached timeline diagram from starting point of “organ offer” to end-point of “transplant surgery.” The timeline provides details on team member roles leading up to the moment of transplant.
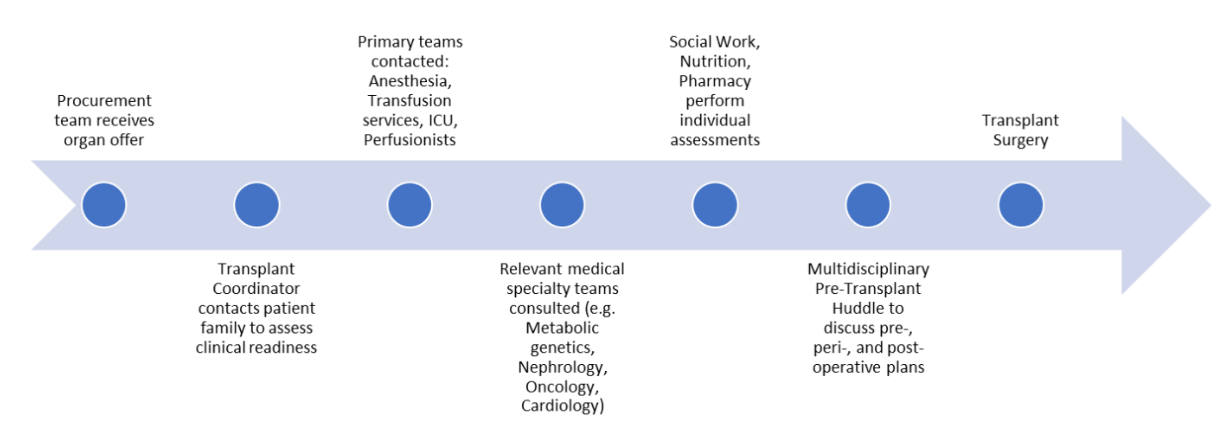
Results: Starting at the time of the organ offer, the procurement coordinator, transplant coordinator (a Nurse Practitioner who provides clinical care for the waitlisted patients), and surgical fellow remain in close communication. Real time updates regarding the donor procurement time, time of organ arrival, recipient OR time, and specific patient needs are efficiently shared between these team members. The transplant coordinator activates a prepared plan that has been individualized for each waitlisted patient. This "care coordination" plan is shared and accessible to all care team members in the patient's Epic chart. It involves details pertaining to transport/travel at time of offer, specialist consults needed at time of transplant, special anesthesia or central access needs, and any social work considerations. Based on this care coordination plan, relevant medical specialties are notified of the transplant offer, and are invited to the pre-transplant huddle. The “Pre-Transplant Huddle” involves representatives from surgery, hepatology, anesthesia, perfusionists, OR staff, and any other specialists specific to the transplant case. The forum allows for open dialogue regarding pre-, peri-, and post-operative plans. Details of the donor organ, timing of donor and recipient OR times are reviewed. This discussion space also invites contributions from any relevant medical specialties (e.g. metabolic considerations for underlying metabolic diseases, need for intra-op CRRT, potential cardiac events).
Conclusion: Our model of task delegation amongst distinct members of the transplant team facilitates efficient and open communication, thereby supporting positive postoperative outcomes. The Pre-Transplant Huddle provides a platform for interdisciplinary discussion for shared decision-making between pertinent specialists, for example in cases necessitating intraoperative CRRT, metabolic protocols, or joint cardiac cases.
[1] care coordination
[2] transplant surgery
[3] perioperative care
[4] transplant waitlist
[5] transplant coordinator
[6] donor offer
[7] liver transplant
[8] multidisciplinary team
[9] organ procurement
[10] transplant call