Left behind – Kidney transplant listing patterns in adolescents and young adults
Margret Bock1, Eric G Benz1, Joseph Fishbein2, Priya Verghese2.
1Pediatrics, University of Colorado, Aurora, CO, United States; 2Pediatrics, Northwestern University, Chicago, IL, United States
Adolescent and young adult (AYA) kidney transplant (KT) recipients have more graft loss compared to other age groups, often during the period when they transition from pediatric to adult care. Academic societies including the American Academy of Pediatrics and the American Society of Transplantation have published guidelines and educational tools to ensure effective care transitions. We aimed to investigate whether patterns in access to transplantation in AYA KT recipients have changed since the adoption of transition to adult care curricula in many transplant programs across the United States.
We examined 51,728 KT patients who were waitlisted by age 30 between 2002 and 2022, as recorded in the Scientific Registry of Transplant Recipients (SRTR) database. We then evaluated 48,436 patients who received kidney transplants age 30 and younger. We generated frequency tables of age at transplant and visualized the distribution with histograms. To model the age-related trends in frequency, we fit a quadratic regression model for counts, using age and age-squared as predictors. Using this model predicted values were calculated at each age, which we then compared to the observed values. Using a one-sample t-test, residuals were tested within our ages of interest to see if they significantly differed from 0.
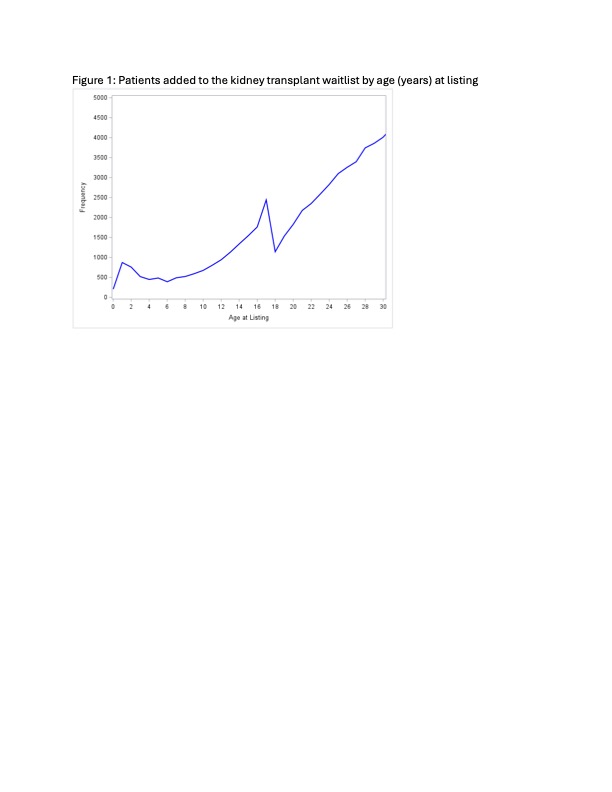
The number of patients listed for KT per year of age in our cohort peaked at 17 years of age, decreased at 18 and 19 and then returned to a steady increase at age 20 years (Figure 1). In our cohort, the absolute number of patients receiving KTs rose at each year of age until peaking at 17yo (N = 2053). Despite prevalence of new ESRD diagnoses historically remaining stable, the number of patients receiving kidney transplants at 18 and 19 years old decreased until age 20, then steadily increased again through the remainder of our cohort (Figure 2a). A similar “age-dip” was found in AYA recipients of deceased donor KTs but was not seen in recipients of living donor KTs (Figure 2b). This “age-dip” pattern was observed regardless of recipient sex (Figure 2c).
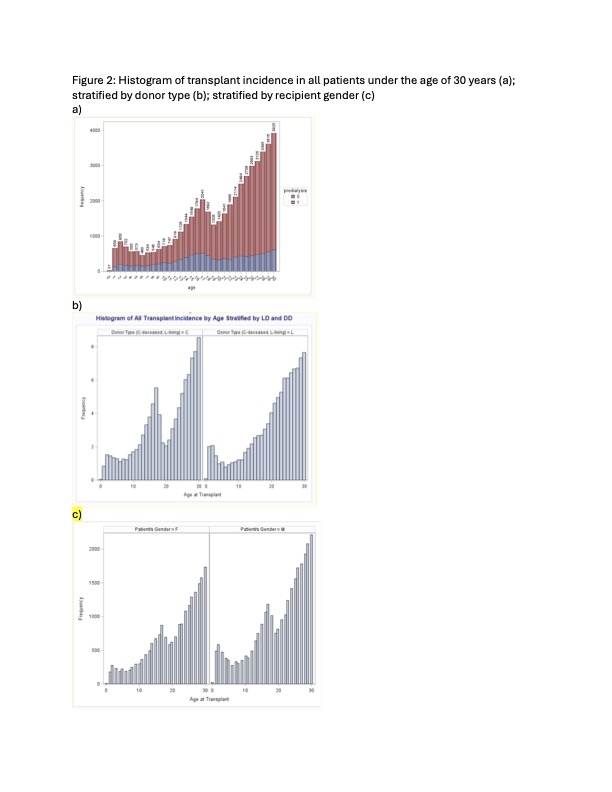
Despite efforts to improve transitions to adult from pediatric KT care, and potentially mitigating allograft loss during that period, 18–20-year-old AYA patients are listed for transplant less frequently and receive fewer deceased donor transplants than their younger and older peers. We propose further studies be completed to determine whether there is hesitation by pediatric and adult transplant providers to transplant this age group based on known risk for allograft loss, and if so, why having a living donors may mitigate this finding.
[1] Kidney
[2] Transplant Listing
[3] Adolescence
[4] Adherence
[5] Transition