2 year follow-up of a pediatric kidney transplant recipient from a donor with known autosomal dominant polycystic kidney disease
Ben Reynolds1, Vladyslav Shumeyko1, Rosalyn Ardill2.
1Paediatric Nephrology, Royal Hospital for Children, Glasgow, United Kingdom; 2Royal Hospital for Children and Young People, Edinburgh, United Kingdom
Introduction: Use of extended-criteria donors in transplantation is a valid strategy to reduce overall waiting times for organs. Though long wait times in paediatrics are rarer, the number of children on the deceased donor list hit a record high following the Covid-19 pandemic.
Methods: We report a male patient with a background of posterior urethral valves, early onset end stage kidney disease, initial renal graft aged 3 years, with subsequent graft failure at the age of 9 years secondary to bladder dysfunction and a massive bladder diverticulum. He was recommenced on haemodialysis. The graft was removed due to concerns regarding ongoing immunosuppression, and he subsequently became highly sensitised with a panel-reactive antibody count of 100%. Vascular access became problematic and an arterio-venous fistula was formed, which then developed high flow. Imlifidase was considered due to the risk of losing dialysis access, but complicated by the absence of a suitable living donor and inexperience in paediatric patients.
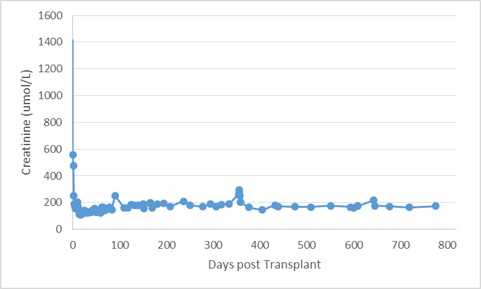
Aged 13, after 4 years on dialysis, he received a deceased brain-death donor kidney from a donor with excellent premorbid kidney function, but a known history of autosomal dominant polycystic kidney disease (ADPKD). The organ was 15cm in length, and full of cysts. After lengthy discussion with the family, the transplant proceeded. Graft function was immediate; serum creatinine stabilised around 160-170umol/litre. There was development of new donor-specific antibody within the first 2 weeks post-transplant, treated with 4 sessions of plasmapheresis and a single dose of rituximab. Donor specific antibody have been undetectable since.
Results: We report his medium-term outcome. The patient is now 2 ½ years post-transplant. There were 3 admissions with urinary tract infection in the first 12 months, but no in-patient admission has been required for over a year. Graft function remains very stable, with latest creatinine of 174umol/L (Figure 1). There have been no symptoms of abdominal pain, or distension from cyst growth. Serial imaging demonstrates a static appearance to the kidney.
Conclusion: Use of a kidney from an ADPKD donor allowed return to school and freedom from multiple medications in a highly sensitised child with diminishing dialysis options. Though an unusual example of extended criteria, this case supports the existing (very limited) literature that ADPKD kidneys can deliver good graft outcomes, and may be considered for challenging cases such as highly sensitised, or urgent transplants.
[1] Extended criteria donor
[2] Allograft survival
[3] Highly sensitised recipient