Succesfull treatment of biliary rhabdomyosarcoma with neo-adjuvant chemotherapy and liver transplantation
Fatma Burcu Belen Apak1, Ceren Kilci1, Pamir Isik1, Fazilet Kayaselcuk2, Mehmet Coskun3, Lale Olcay4, Adem Safak4, Emre Karakaya4, Mehmet Haberal4.
1Pediatric Hematology and Oncology, Baskent University Medical Faculty, Ankara, Turkey; 2Department of Pathology, Baskent University Medical Faculty, Ankara, Turkey; 3Department of Radiology, Baskent University Medical Faculty, Ankara, Turkey; 4Department of General Surgery and Transplantation, Baskent University Medical Faculty, Ankara, Turkey
Introduction: Rhabdomyosarcoma (RMS) is a malignant tumor with striated muscle differentiation, with the biliary tract being an extremely rare primary site (0.5–1.5% of pediatric cases). We report a case of embryonal biliary rhabdomyosarcoma treated with neoadjuvant chemotherapy and liver transplantation.
Case Report: A 2-year-old Moroccan girl presented with a progressive abdominal mass causing respiratory distress and feeding difficulties. A biopsy in Morocco diagnosed alveolar RMS, and two cycles of VAC chemotherapy (vincristine, actinomycin-D, cyclophosphamide) were given, but the tumor continued to enlarge.
On admission, she had a 20 cm abdominal mass.

Laboratory tests revealed mild anemia (Hb: 9 g/dL), elevated LDH (1031 IU/dL), and uric acid (7 mg/dL), while liver function tests and tumor markers were normal. MRI showed a 240 × 224 × 156 mm hepatic mass extending into the peritoneal cavity, with cystic and solid components. PET-CT demonstrated FDG uptake (SUVmax: 2.3) without distant metastases. A tru-cut biopsy confirmed embryonal RMS.
She received 12 weeks of chemotherapy (vincristine, cisplatin, doxorubicin, cyclophosphamide, actinomycin-D), reducing abdominal circumference from 78 cm to 60 cm. Follow-up MRI showed tumor shrinkage (199 × 195 × 114 mm) with necrosis and hemorrhage, no lymphadenopathy, or peritoneal involvement. She underwent orthotopic liver transplantation from her father following total hepatectomy.
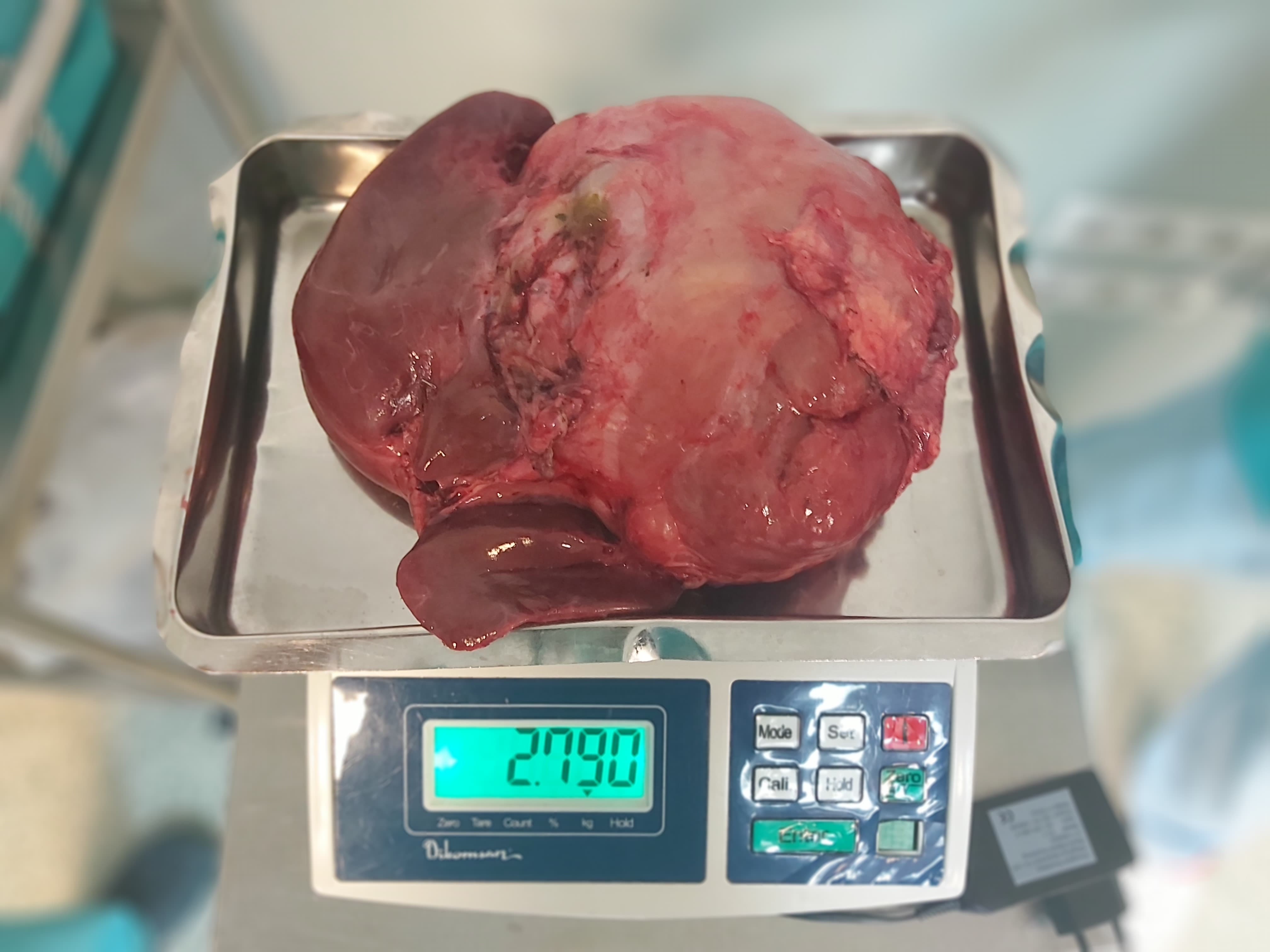
Histopathology of the 37.5 × 19 × 11 cm, 2755 g liver revealed a 20 × 20 × 11 cm tumor. Immunohistochemistry showed desmin, myogenin, and MyoD1 positivity, focal SMA positivity, and S100 negativity, with a Ki-67 index of 2%. She was discharged two weeks post-transplantation without complications, and four additional chemotherapy cycles were planned.
Conclusion: Primary hepatic or biliary RMS is rare. Neoadjuvant chemotherapy can reduce tumor burden, enabling complete surgical resection or transplantation. Embryonal RMS has the best prognosis, whereas alveolar and pleomorphic subtypes are more aggressive. Though no standard guidelines exist, tumor reduction before transplantation appears to be a viable approach.
References:
1. Fuchs J, Murtha-Lemekhova A, Kessler M, Günther P, Fichtner A, Pfeiffenberger J, Probst P, Hoffmann K. Biliary Rhabdomyosarcoma in Pediatric Patients: A Systematic Review and Meta-Analysis of Individual Patient Data. Front Oncol. 2021 Sep 30;11:701400.
2. Chavhan GB, Siddiqui I, Ingley KM, Gupta AA. Rare malignant liver tumors in children. Pediatr Radiol. 2019 Oct;49(11):1404-1421.
3. Kebudi R, Görgun O, Ayan I, Coşar R, Bilgiç B. Rhabdomyosarcoma of the biliary tree. Pediatr Int. 2003 Aug;45(4):469-71.
[1] biliary rhabdomyosarcoma, liver transplantation, neo-adjuvant chemotherapy