
Breadth of care: Modern treatment options for pediatric portal vein thrombosis
Rebecca Mercedes1, Wenly Ruan1, Shruti Sakhuja1, Peace Dike1, Madelyn Cohen1, Ashley Upton1, Marielle Faraone1, Kelby Fuller1, Anna Banc-Husu1, Paula Hertel1, Krupa Mysore1, Elizabeth Tessier1, Sanjiv Harpavat1, Henry Shiau1, Naseem Ravanbakhsh1, Dan Leung1, Ben Shneider1, Jonathan Gross1, Doug Fishman1, Alex Chau1, Young Na Lee-Kim1, Sarah Sartain1, Clay Cohen1, John A Goss1, J Alberto Hernandez1, Thao Galvan1.
1Texas Children's Hospital, Baylor College of Medicine, Houston, TX, United States
Purpose: Extrahepatic portal vein obstruction contributes to the majority of cases of portal hypertension in the pediatric population. Our study aims to provide an overview of surgical and catheter-based techniques used to correct portal hypertension in our cohort of pediatric patients after the establishment of a multidisciplinary consortium dedicated to state-of-the-art interventions.
Methods: Using sonography, catheter-directed interventions, and surgery to include liver transplantation, our center has developed a multidisciplinary approach to manage pediatric patients with portal vein thrombosis (PVT). In our retrospective cohort, we describe 5 cases highlighting different modalities from the use of catheter-based venoplasty, the modified Sugiura, the distal splenorenal shunt, and portal vein reconstruction to address PVT, up to and including liver transplantation.
Results:
Case A: An 11 yo pt who previously had an UVC developed PVT complicated by GI bleeding. Using catheter-based venoplasty, the patient underwent successful portal vein recanalization with patent PV 23 months out.
Case B: An 18 yo pt with PVT and splenomegaly underwent splenectomy and modified Sugiura to address her acute upper GI bleed. She later developed superior mesenteric vein thrombus and splenic artery pseudoaneurysms, successfully managed with aneurysm coiling, bowel rest, and therapeutic enoxaparin with no further GI bleeding. She has since safely delivered a newborn and has not rebled.
Case C: A 5 yo pt who previously underwent Kasai procedure for biliary atresia and liver transplant who later developed PVT. This was treated with a surgical distal splenorenal shunt, complicated by shunt thrombosis. Balloon angioplasty and stenting allowed for recanalization, and the shunt remains patent 3 years out.
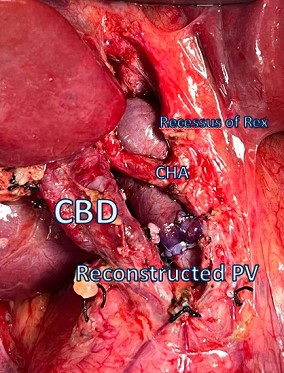
Case D: An 8 yo pt presented with massive gastrointestinal bleeding which was unsuccessfully temporized by embolization. Her PVT was managed with total reconstruction by portal vein excision followed by physiologic reconstruction using internal jugular vein. Her reconstruction remains patent 24 months out with resolution of her thrombocytopenia.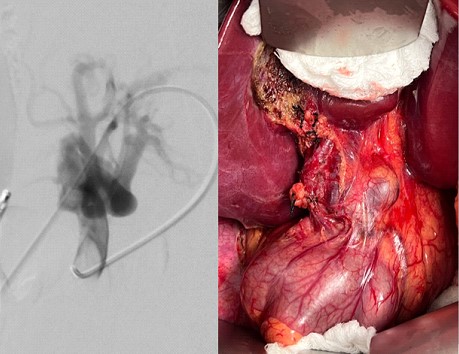
Case E: A 9 mo old previously premature pt with history of UVC and omphalitis presented with a second GI bleed. EGD demonstrated grade 3 gastric varices. US demonstrated cavernous transformation of PV and no intrahepatic portal branches. IR venogram and attempted venoplasty was unsuccessful, and because there was no communication between the left and right portal veins, the pt will be evaluated for liver transplantation.
Conclusions: Sequalae of unmanaged PVT in pediatric patients can lead to debilitating physiologic consequences. Using novel surgical and endovascular techniques in a concerted effort by a devoted multidisciplinary team, we have identified various approaches to correcting portal hypertension in our pediatric cohort, including liver transplantation.
[1] Portal Vein Thrombosis
[2] Catheter Directed Therapy
[3] Multidisciplinary