Prognosis factors and surgical management of biliary complications after pediatric liver transplantation in la Fundacion Cardioinfantil-laCardio, a specialized, high-complexity center in Bogotá, Colombia
Jairo Rivera-Baquero1, Nathaly Ramírez1, Daniela Sánchez-Santiesteban1.
1Transplant Unit, Fundación Cardioinfantil-Instituto de Cardiología, Bogotá D.C, Colombia
Background: Biliary complications (BCs) remain a significant challenge in pediatric liver transplantation (LT), with reported incidence rates ranging from 10%-35%. This study aimed to assess the incidence and prognosis factors of BCs following pediatric LT at a specialized, high-complexity center in Bogotá, Colombia.
Methods: A retrospective analysis was conducted on 392 pediatric patients who underwent Liver Transplant between October 2007 and March 2025 at Fundación Cardioinfantil - laCardio. We described demographic, clinical, and surgical characteristics, as well as the cumulative 4-year incidence of BCs and their management. Bivariate and multivariate logistic regression models were used to explore associations with the development of BCs within a 4-year follow-up period. This study was approved by the Ethics Committee at Fundación Cardioinfantil–Instituto de Cardiología (CEIC-110-2025).
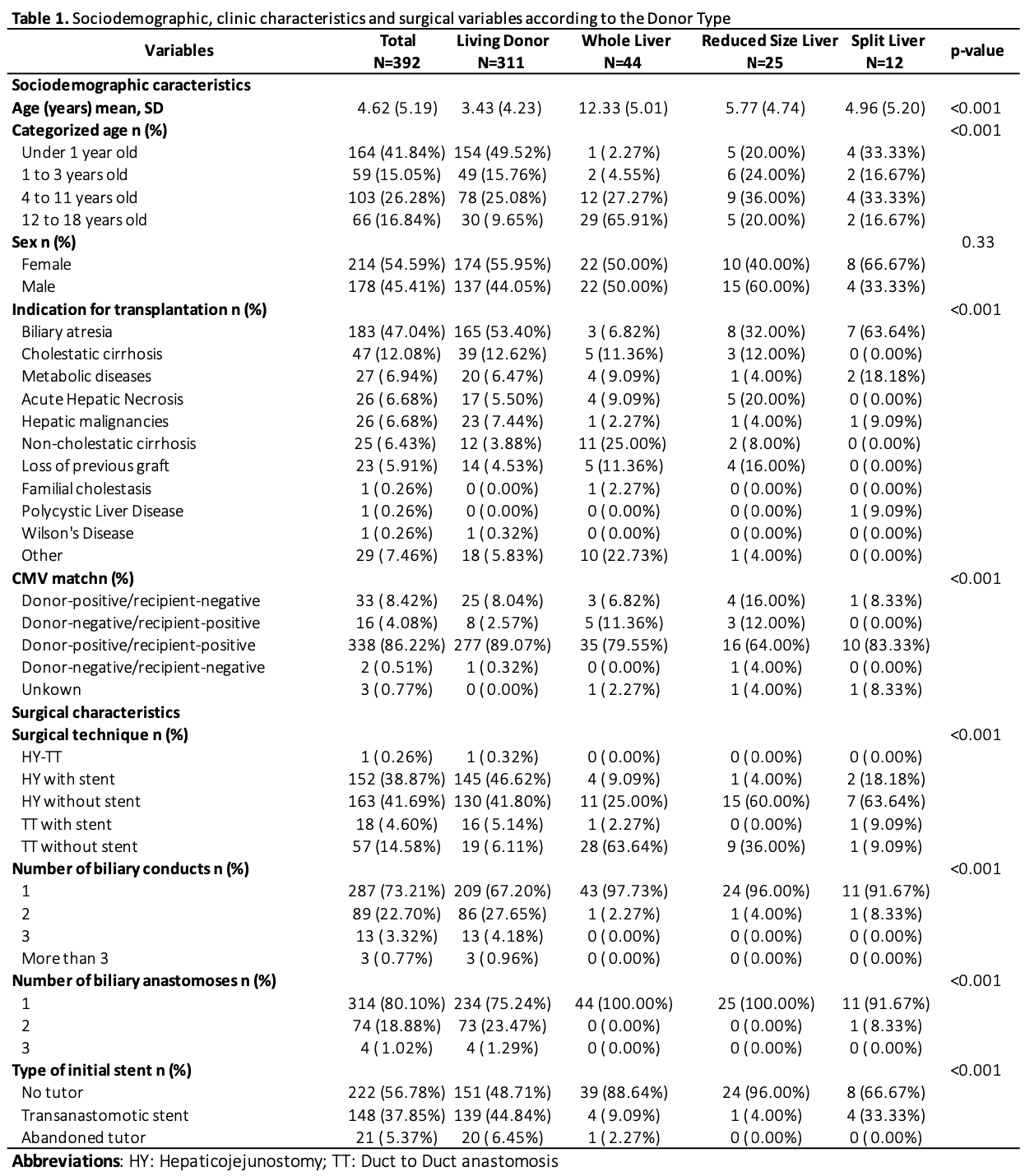
Results: Of the 392 patients, 54.59% were female, with a mean age of 4.62 years (SD, 5.19). The leading indication for LT was biliary atresia (47.04%), most patients received grafts from living donors (79.33%), and the most common surgical technique was hepaticojejunostomy (HY) without stent (41.69%). A single bile duct was identified in 73.21% of patients, and one biliary anastomosis was performed in 81.10% of patients. Further details on the patients’ sociodemographic, clinical and surgical variables are shown in Table 1. The median hospital stay was 24 days (IQR: 14), and the critical care stay was 7 days (IQR: 7).
During follow-up, 116 patients (29.59%) developed BCs. Among these, anastomotic strictures were observed in 46.96% of patients and anastomotic fistulas in 41.74% of patients, accounting for 88.79% of all BCs. A total of 49 patients (12.50%) developed a fistula within the first 30 days post-transplant. Most BCs (68.97%) occurred before 2021, and the most frequent approach to manage BCs was percutaneous-only, serial bioplastics (35.34%), followed by ERCP (16.38%).
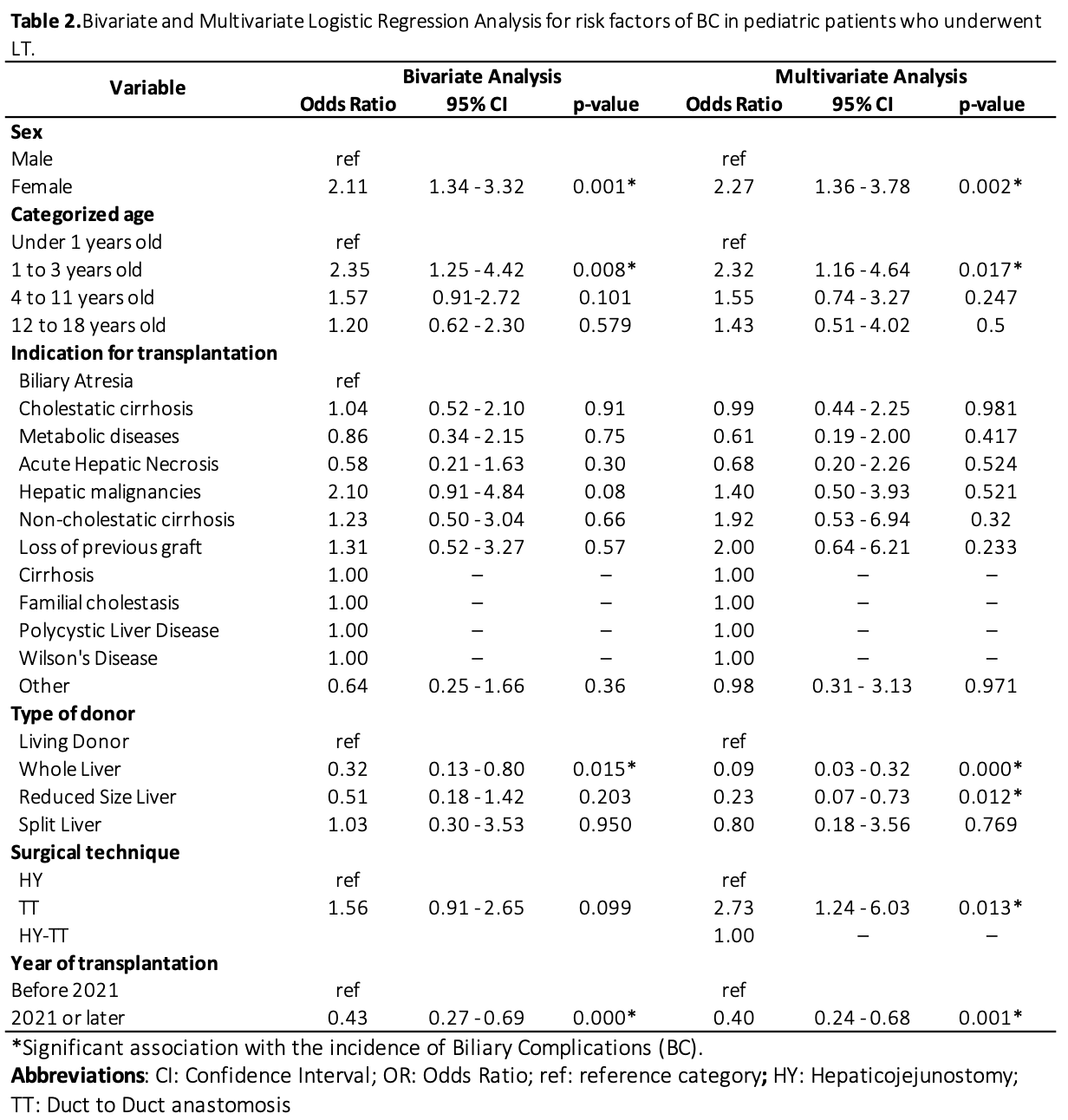
In bivariate analysis, female sex, age, type of donor and year of surgery were significantly associated with BCs. In multivariate analysis, female sex (OR:2.27, 95%IC:1.36-3.78), age between 1-3 years old (OR:2.12 95%IC:1.16-4.64) and duct-to-duct anastomosis (OR:2.73, 95%IC:1.24-6.03) were associated with higher odds of developing BCs. Whole liver graft (OR:0.09, 95%IC:0.03-0.32), reduced-sized liver graft (OR:0.23, 95%CI:0.07-0.73) and surgery performed since 2021 (OR:0.40, 95%CI:0.24-0.68) were associated as protector factors. Full model results are presented in Table 2.
Conclusions: BCs continue to pose a significant challenge in pediatric liver transplantation. The associations observed between sex, surgical technique and donor type indicate that these factors may serve as critical considerations in the planning and execution of pediatric LT. The reduction in BCs observed since 2021 may reflect the adoption of exteriorized catheters through biliary-enteric anastomosis.
[1] Pediatric liver transplantation
[2] Biliary complications
[3] Prognostic factors
[4] Retrospective cohort study