Fungal foes: A decade of antifungal practices in pediatric lung transplant
Sruti Nadimpalli2, Jake Brockmeyer3, Erica Wong3, Nicholas Avdimiretz1.
1Department of Pediatrics, Division of Respiratory Medicine, University of British Columbia, Vancouver, BC, Canada; 2Department of Pediatrics, Division of Infectious Diseases, Stanford University, Stanford, CA, United States; 3Department of Pharmacy, Stanford University, Stanford, CA, United States
Purpose: Fungal infections represent a significant risk in the post-organ transplant population, and lung transplant patients are at high risk due to degree of immunosuppression, antecedent colonization of the respiratory tract, and underlying pre-transplant lung disease. Approaches to pre- and post-transplant antifungal prophylaxis in this vulnerable population vary widely, with each antifungal class having limitations in the form of toxicities and medication interactions. Despite the emergence of novel antifungals over the last decade, data on the optimal use and duration of antifungal therapy in lung transplant patients remain scarce in the modern era.
Methods: This retrospective study reviewed antifungal use in pediatric lung transplants from 2014 to 2024. Heart transplant and heart-lung transplant recipients <18 years at the time of transplant were included. Demographic and clinical data collected included age/sex, date of transplant, organ type(s), induction and maintenance immunosuppression, and antifungal agent(s) and dosing both before and after transplantation. Clinical outcomes including death, acute rejection (either clinically identified or biopsy-confirmed), and chronic lung allograft dysfunction were recorded. Microbiologic data collected included organisms isolated by culture from the respiratory tract either before or after transplant.
Chi-square analysis was utilized to identify associations between antifungal duration, post-transplant colonization, rejection, and pre- and post-transplant fungal growth.
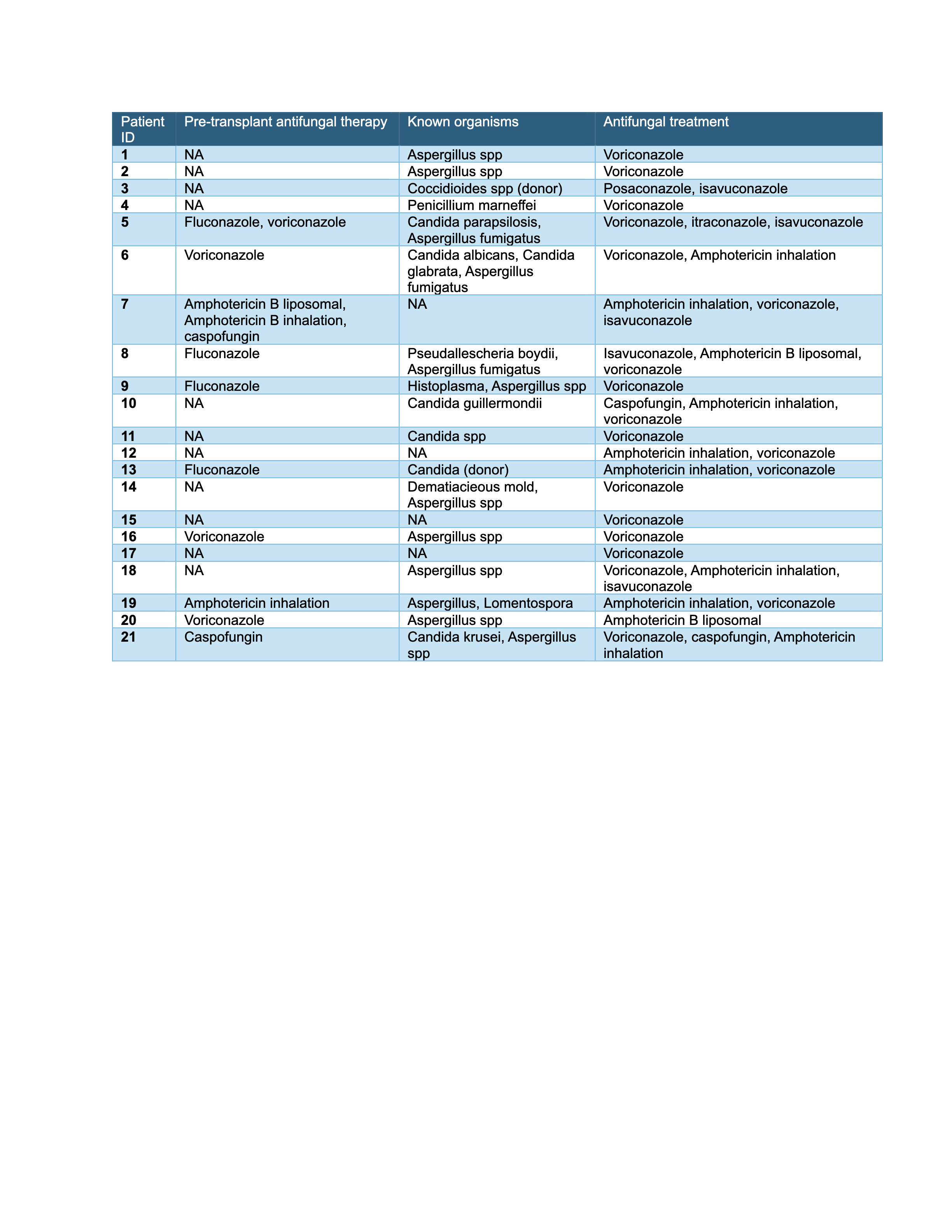
Results: In all, 21 patients met inclusion criteria and were reviewed: 15 had bilateral lung transplants, and 6 underwent combined heart-lung transplantation. Indications for transplant included cystic fibrosis (n=10), pulmonary hypertension (n=7), pulmonary fibrosis (n=2), bronchiectasis obliterans (n=1) and bronchopulmonary malformation (n=1).
Seventeen patients (81.0%) had microbiologic evidence of fungal colonization or infection after transplant. Of 10 patients initiated on antifungals prior to transplant, 9 (90.0%) had positive fungal cultures post-transplant, including Candida, Scedosporium, Histoplasma, and Aspergillus species.
There was no significant association between likelihood of positive pre-transplant fungal culture and likelihood of fungal infections after transplant (χ² = 0.88; p = 0.35). No association was found between pre-transplant fungal culture and likelihood of discontinuation of antifungal therapy (χ² = 1.29; p = 0.26). Patients with rejection episodes were less likely to have their antifungal prophylaxis discontinued (5/16, 31.3%) compared to those who did not experience rejection (4/5, 80.0%), and this difference approached significance (χ² = 3.697; p = 0.054).
Conclusion: This single-center study suggests that antifungal prophylaxis strategies remain variable across lung transplant recipients irrespective of pre-transplant fungal colonization status. Post-transplant fungal infection was also common despite initiation of antifungal prophylaxis after transplant. Practice variation also exists with regard to antifungal choices. These data underscore the need for further multicenter analyses and consensus guidelines for antifungal prophylaxis as indications for lung transplant evolve and new antifungals become widely available.