Normothermic machine perfusion in pediatric DCD liver: First attempt in China
Jianjun Zhu1, Dongwei Xu1, Lei Xia1, Qiang Xia1.
1Liver Surgery, Renji Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, People's Republic of China
Introduction: Normothermic machine perfusion (NMP) has emerged as one of the most prominent advancements in liver transplantation. This technology demonstrates significant improvements in graft quality for adult liver grafts derived from donation after circulatory death (DCD). However, its application in pediatric DCD livers remains scarcely documented. To address this knowledge gap, we conducted a pioneering attempt to implement NMP preservation for a pediatric DCD liver graft.
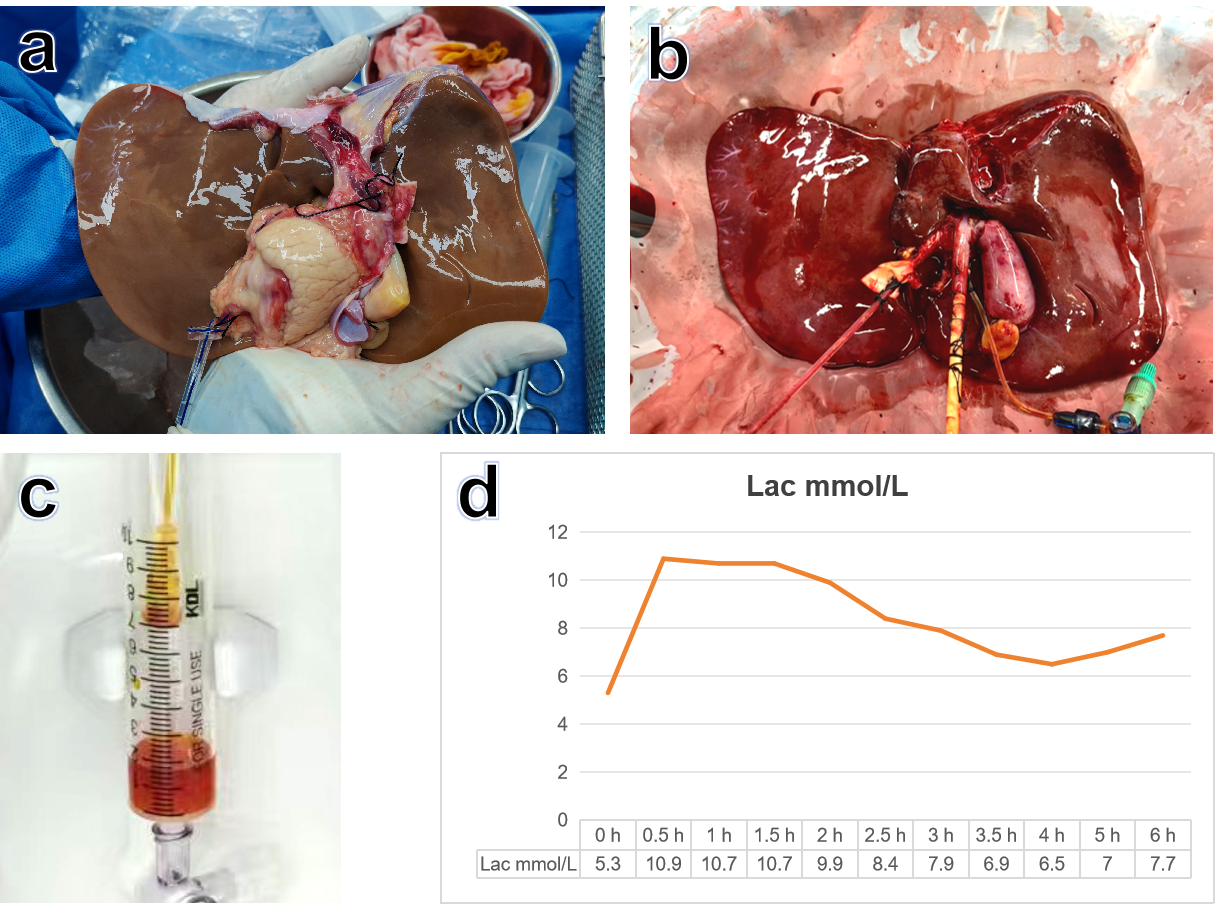
Methods: The donor was a 4-year-old male who succumbed to hypoxic-ischemic encephalopathy after 12 days of ICU hospitalization. Organ procurement followed DCD protocols, with warm ischemia time exceeding 20 minutes and cold ischemia time lasting over 9 hours (Figure 1a). The hepatic graft weighed 600 grams. A NMP system was employed for 6 hours using a perfusate composed of red blood cells (Figure 1b). Perfusate gas analysis was monitored at 30-minute intervals. Continuous macroscopic evaluation included assessments of hepatic coloration, parenchymal texture, and bile production volume. Perfusion dynamics (pressure and flow rate) were dynamically adjusted based on real-time monitoring data.
Results: The liver graft quality was comprehensively evaluated according to established VITTAL criteria and ultimately deemed unsuitable for transplantation based on the following markers of suboptimal functional viability:
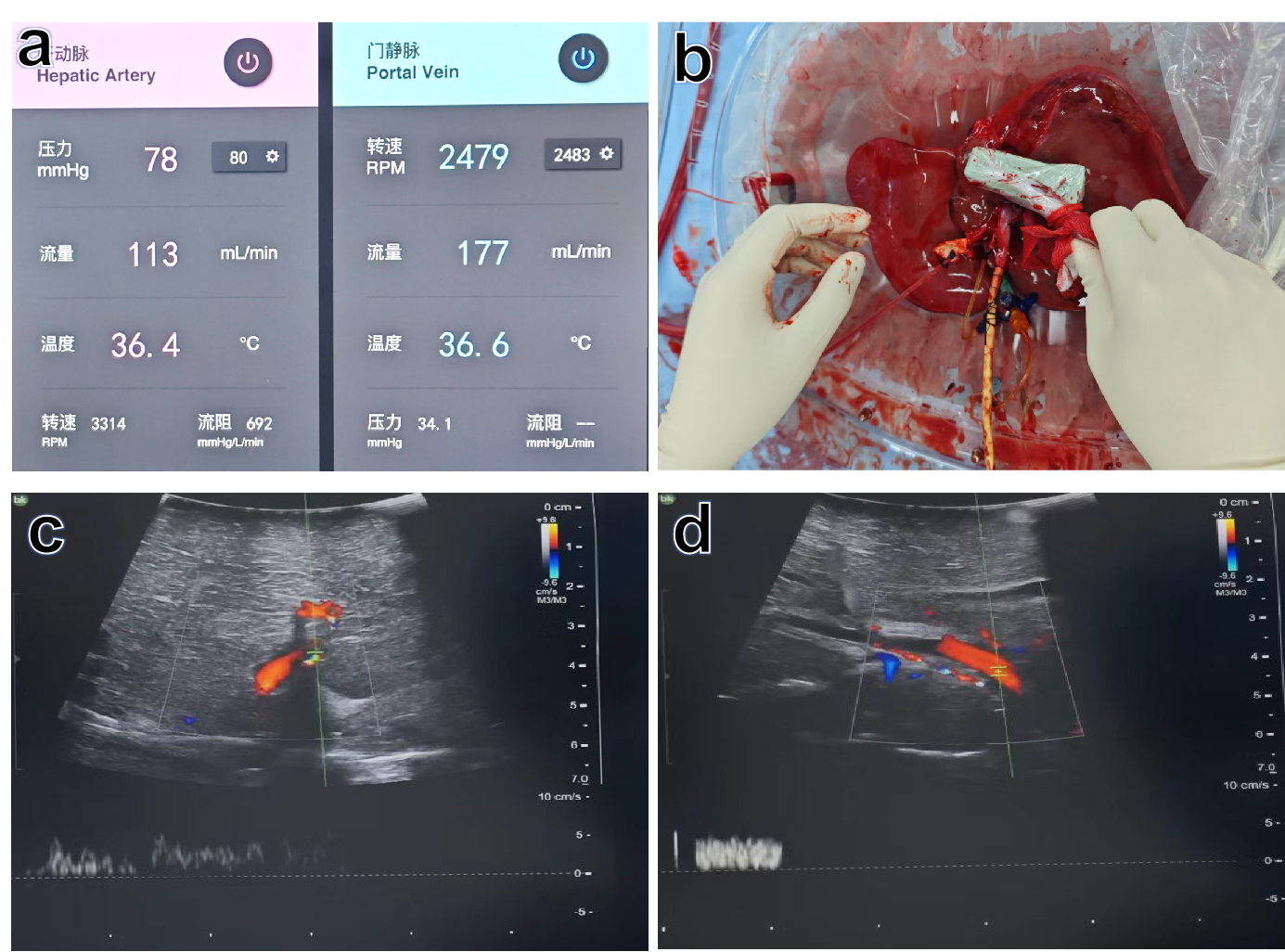
Conclusion: This is the first reported case of NMP applied to a pediatric DCD donor liver in China. After 6 hours of NMP preservation, the graft demonstrated suboptimal functional parameters and viability indicators, rendering it unsuitable for transplantation due to combined injuries from prolonged warm and cold ischemia times.
Given the critical shortage of pediatric donor livers and the technical complexities associated with NMP in this population, pediatric NMP applications remain exceptionally rare worldwide. Our study represents a preliminary exploration in this challenging field, aiming to establish technical protocols, optimize perfusion parameters, and ultimately expand the pediatric donor pool through improved organ resuscitation strategies.
[1] normothermic machine perfusion
[2] donation after circulatory death
[3] pediatric donor liver