Neonatal acute liver failure secondary to enteroviruses: Outcome with or without liver transplantation
Sharath Manya1, Anil Dhawan1, Anita Verma2.
1Paediatric Liver, Gastroenterology and Nutrition Centre, King’s College Hospital NHS Trust, London, United Kingdom; 2Department of Infectious Sciences, King’s College Hospital, London, United Kingdom
Introduction: Neonatal acute liver failure (ALF) is a rare but fatal condition with a mortality of up to 50%. Amongst the known common causes are herpes virus, metabolic diseases, gestational alloimmune liver disease (GALD), and ischaemic injury. Up to 40% of cases have an unknown etiology. Human enterovirus (HEV) infections are common in neonates, with serious clinical manifestations including myocarditis, meningoencephalitis and more rarely can cause ALF with a fulminant course. The aim of this study was to summarize the clinical characteristics of neonates with severe HEV leading to ALF in our centre, to provide experience on management and outcome with and without liver transplantation(LTX).
Methods: Patients with ALF and HEV infection were identified from our clinical database. The demographics, clinical presentations, laboratory data and outcomes were collected from electronic medical and laboratory databases. Viral testing was done by real-time PCR in blood and respiratory secretions. Serotyping of HEV was done from virology reference laboratory.
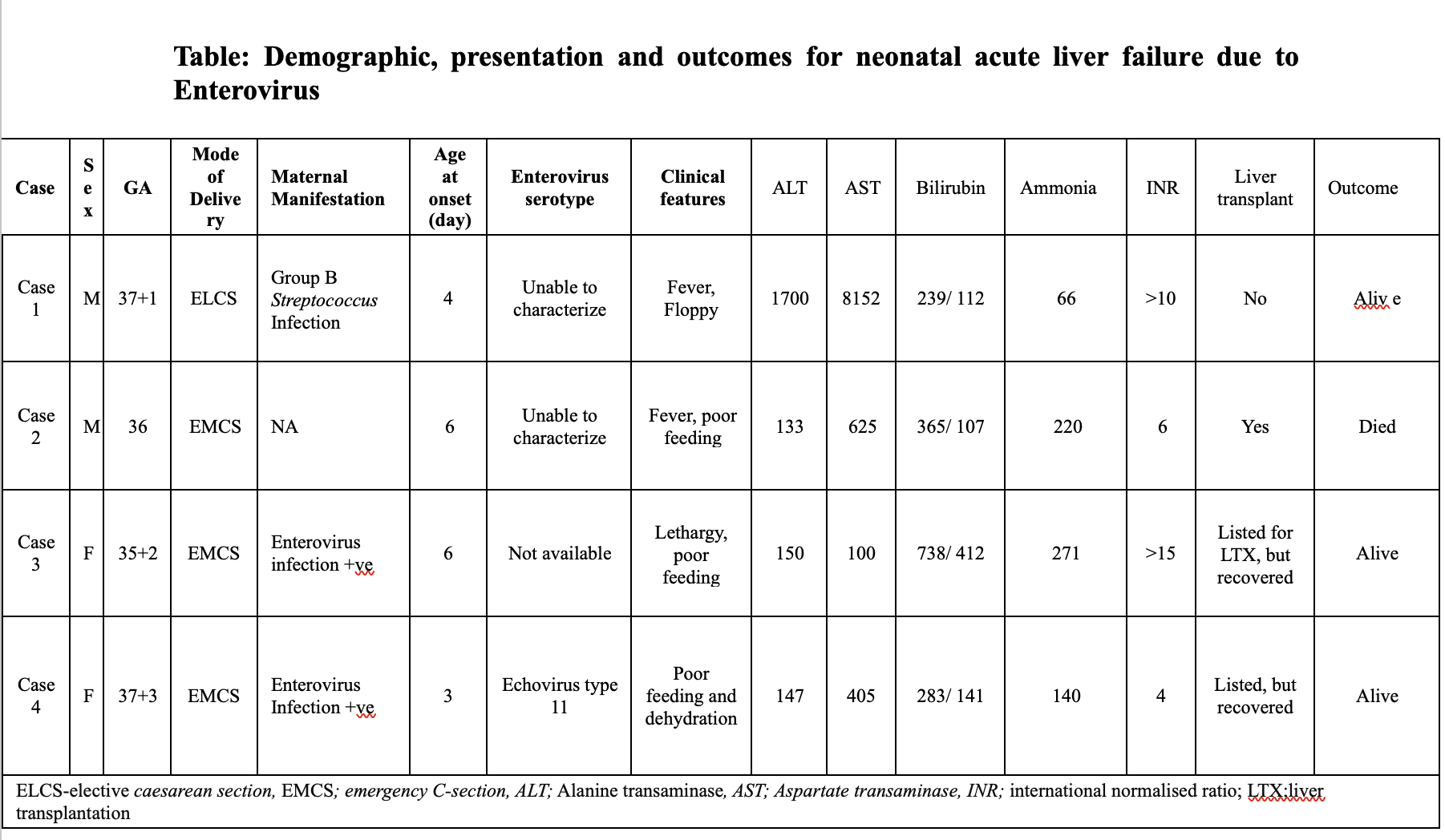
Results: Four cases of neonatal ALF due to HEV (Table 1) were identified between Oct 2022 – Mar 2024. Mothers tested positive for HEV in two cases during the perinatal period. All neonates were born via C-section and all presented with ALF at our institution. Extensive investigation was done to exclude other causes of ALF and immunodeficiency. Only one child had a concomitant diagnosis for GALD. Severe coagulopathy with low fibrinogen was seen in all cases requiring regular blood products. All children were managed supportively in our critical care unit with ventilation and renal replacement therapy. All patients received intravenous immunoglobulin (IVIG) and antimicrobials. Three patients were listed for LTX but only one received LTX. However, this infant died post LTX because of multiple post-LTX complications and fungal infection. All other neonates survived with near normalization of liver function.
Conclusions: Our data suggests an increasing incidence of HEV neonatal ALF associated with severe coagulopathy fulfilling criteria for LTX. The decision for LTX in this setting can be challenging, as there is little evidence on outcomes in these neonates. We recommend that HEV testing should be added to the diagnostic algorithm for all neonatal ALF to help in management. Newer antiviral agents for HEV are under investigation but more clinical evidence for its use is still required.
[1] Acute Liver Failure
[2] Neonates
[3] Neonatal acute liver failure
[4] Enterovirus
[5] Liver transplantation